Lingulectomy removes infection when antibiotics fail
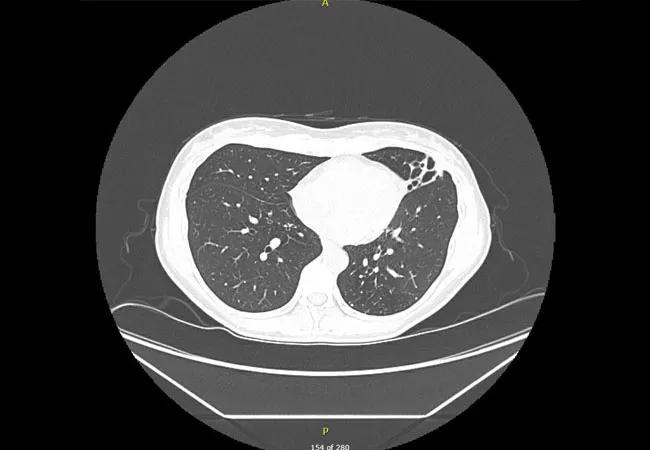
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8013aece-2d96-4e65-b94c-42b9ad8ae1e8/21-PUL-2288127-CQD-Complex-Case-650x450-CT-Chest-HERO_jpg)
21-PUL-2288127 CQD Complex Case 650×450 CT Chest HERO
By Lucileia Johnson, MD; Michelle Biehl, MD; Usman Ahmad, MD; and Sanjay Mukhopadhyay, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 49-year-old woman was diagnosed with lingular bronchiectasis via CT scan and pulmonary clarithromycin-susceptible Mycobacterium avium complex (MAC) infection via bronchoscopy. Alpha-1 antitrypsin was normal. Rheumatoid factor was negative. Immunoglobulins were normal. Sweat test was negative.
She was treated with azithromycin, rifampin and ethambutol three times per week. However, seven months later, sputum smear and culture showed no microbiological response. After one month of daily dosing, sputum smear and culture were still positive for Mycobacterium avium-intracellulare.
Because the patient could not tolerate daily dosing, she was returned to treatment three times per week, adding inhaled amikacin. One month later she developed mild sensorineural hearing loss.
Despite ongoing treatment, sputum cultures remained positive. Nine months later, all medications were stopped due to side effects — including fatigue, tinnitus and hearing loss — and the inability to clear cultures. However, due to worsening symptoms, treatment with azithromycin, rifampin, ethambutol, clofazimine and amikacin were resumed a few months later.
After six months, due to side effects and still no microbiological response, all medications again were stopped and the patient was referred to Cleveland Clinic’s Nontuberculous Mycobacteria (NTM) Center for refractory, macrolide-resistant MAC infection. At that time, a CT scan revealed increased left-lung-predominant, small, clustered nodules and lingular-predominant bronchiectasis, most likely due to worsening infection.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f328ace2-1bbb-40a1-81c9-784d9c99baa2/21-PUL-2288127-CQD-Complex-Case-850x768-CT-Chest-INSET_jpg)
CT scan showing increased left-lung-predominant, small, clustered nodules and lingular-predominant bronchiectasis.
After talking to the patient, reviewing her CT scan and repeating the sputum culture, the patient was referred to thoracic surgery. Six weeks prior to surgery, she was started on oral moxifloxacin, clofazimine, bedaquiline and intravenous aminoglycoside. She underwent robotic, video-assisted thoracoscopic lingulectomy, with pathology showing necrotizing granulomatous inflammation and acid-fast bacteria.
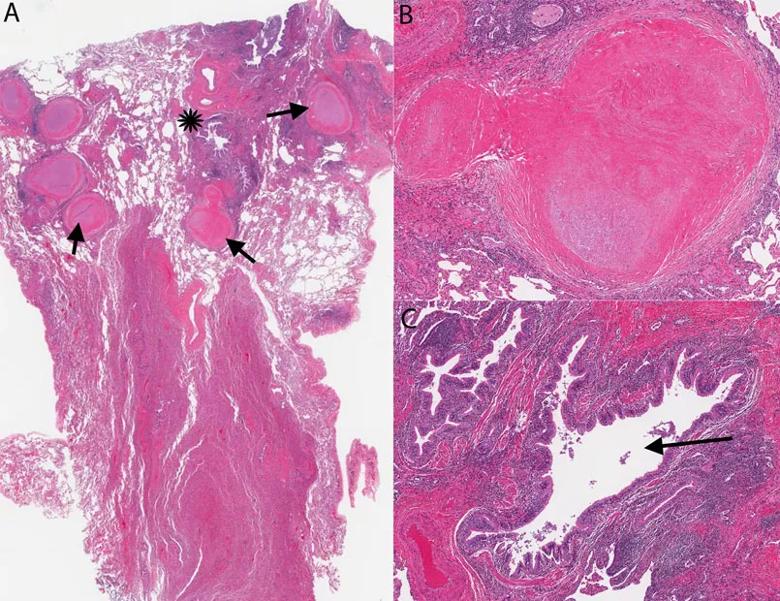
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ff8858e5-6d9a-43d8-8f59-2b72c7a66015/21-PUL-2288127-CQD-Complex-Case-850x620-fig-2-INSET_jpg)
Photomicrographs from the lingulectomy specimen. A. Multiple nodules are evident at low magnification (arrows). These are necrotizing granulomas. An inflamed airway is marked by an asterisk. B. Necrotizing granuloma at higher magnification. C. Markedly inflamed airway (arrow) [All images: hematoxylin-eosin stain].
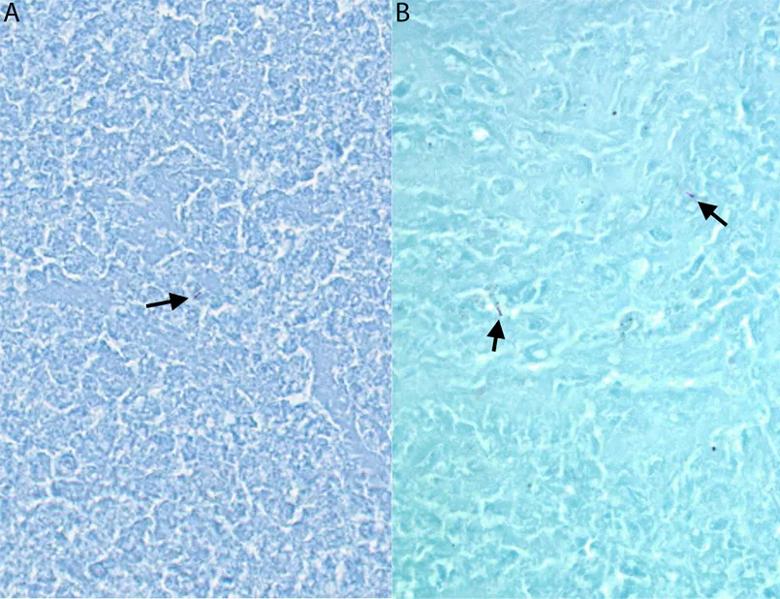
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f2eb7149-4761-4967-98e5-d8e4a8ef8c10/21-PUL-2288127-CQD-Complex-Case-850x618-fig-3-INSET_jpg)
A, B. Mycobacteria (acid-fast bacteria, arrows) within the necrotizing granulomas [Ziehl-Neelsen stain].
Four weeks postop she was transitioned to amikacin liposome inhalation suspension (ALIS). Currently she has completed 24 weeks of bedaquiline and is completing 12 months of ethambutol, clofazimine and ALIS. Since surgery, her sputum cultures have been negative.
Optimal management of refractory NTM infection requires experience and teamwork. The patient in this case improved after lingulectomy. Her outcome was excellent thanks to the collaboration of a multidisciplinary NTM team, including specialists in pulmonology, infectious disease, pathology and thoracic surgery.
Advertisement
All authors are staff at Cleveland Clinic. Lucileia Johnson, MD, is in the Department of Infectious Disease. Michelle Biehl, MD, is in the Department of Critical Care Medicine. Usman Ahmad, MD, is in the Department of Thoracic and Cardiovascular Surgery. Sanjay Mukhopadhyay, MD, is Director of Pulmonary Pathology.
Advertisement
Advertisement
Screen patients seeking care for chlamydia, gonorrhea
Researchers have developed immunoprofiles for an emerging disease with a mortality rate as high as 27%
Findings from one of the first published case series
Don't discount this crucial step
EBUS-TBNA found safe and effective
How to spot the rare infection
Not all lung nodules are malignant
An uncommon condition in a 41-year-old man