Some cases of AAA are still best served by open repair
The benefits of endovascular repair of abdominal aortic aneurysm (EVAR) are well established, and Cleveland Clinic is an avid user of EVAR in appropriately selected patients. Yet it remains true that EVAR is not the best choice for all patients and all cases, and EVAR failure is a reality that high-volume vascular surgery programs continue to see.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cleveland Clinic has the world’s largest experience in treating failed endovascular repairs,” says Department of Vascular Surgery Chair Sean Lyden, MD. A review of that experience suggests that most cases of failed EVAR can be attributed to one of a handful of causes. This short post illustrates those causes with a collection of images from recent cases encountered among patients presenting to Cleveland Clinic for management of failed EVAR.
“In our experience, EVAR failure is most often due to poor planning or simple nonadherence to the instructions for use for the endograft device,” says Cleveland Clinic vascular surgeon Francis Caputo, MD.
The CTs below present cases in point. They are from patients with aneurysm necks between 30 and 32 mm, yet their aneurysms were repaired endovascularly with some of the largest devices available, with diameters of 36 mm. Over time, this mismatch resulted in neck dilation, causing aneurysmal degeneration and slippage of the devices. While the effect appears modest in the coronal views in the top row, the sagittal views below show that the grafts have become so crumpled that they are beyond endovascular salvage.
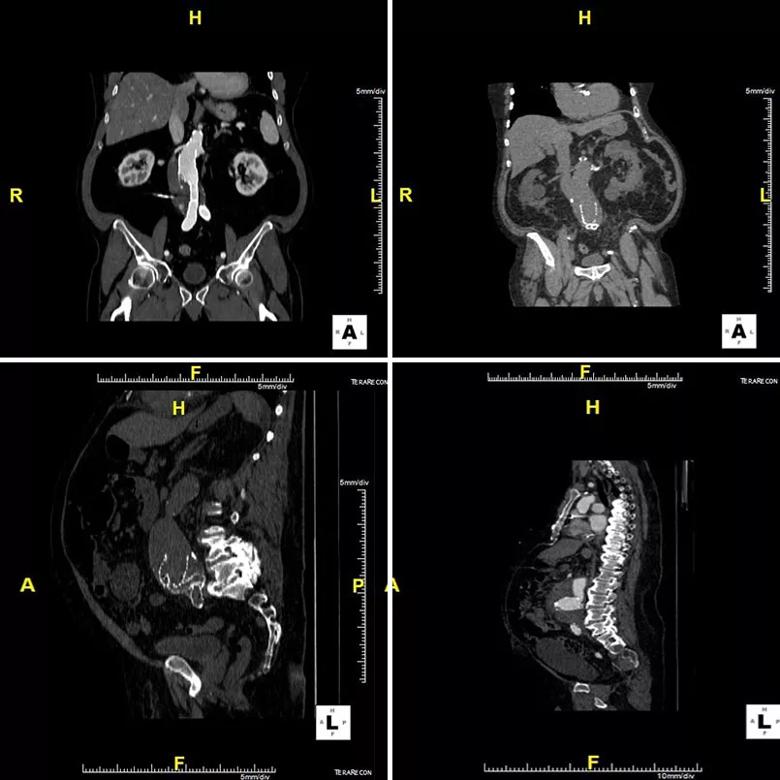
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a40503df-a931-4911-8c3a-e93acd1e9495/18-HRT-5576-failed-EVAR_-Inset-1_jpg)
Durability was a recognized limitation of early endografts, and while next-generation devices have been designed to address durability problems, the success of these efforts is not yet known.
“In our practice, we still encounter degeneration with older endografts, such as fabric tears and fabric absorptions,” observes Dr. Caputo, who supplied the photos below as examples. He notes that the photo on the right reveals just how thin device fabric can become.
Advertisement
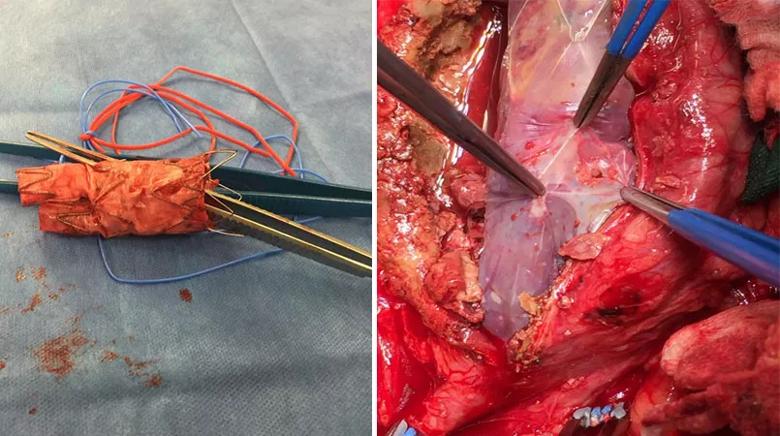
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/094a9004-e4bd-49d0-a648-6c13e9b3d5ea/18-HRT-5576-failed-EVAR_Inset-2_jpg)
“Durability issues are surfacing even with some newer devices, too, as we have seen in some of the trials of new EVAR devices in which we participate,” Dr. Caputo says. An example of a newer device that required removal is shown below.
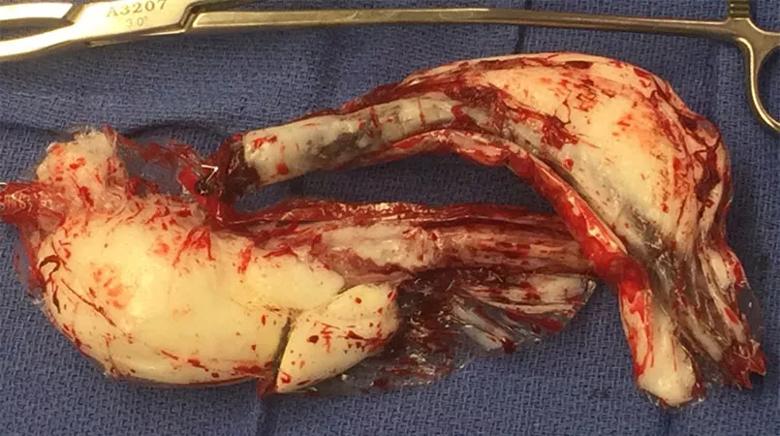
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9e5bc860-8c42-40c0-ae2c-a4fb7e367efc/18-HRT-5576-failed-EVAR_Inset-3_jpg)
One side effect of the growth of EVAR is that open aortic surgical repairs are being done less and less often. Yet continuing robust experience is key to superior outcomes. “Cleveland Clinic’s vast experience has enabled us to consistently achieve less than 1% mortality with open first-time aortic surgery, which compares favorably with Medicare data suggesting a national rate of 4% to 5%,” notes Dr. Lyden.
Diminishing experience with open aortic surgery extends to training programs, Dr. Caputo adds, with today’s vascular surgery fellows graduating after having done, on average, only 10 open aneurysm repairs a year. While programs like Cleveland Clinic’s are proud to be exceptions to this trend — its fellows graduate with about 80 open aneurysm repairs a year — the broad effect is that experience with open aortic surgery is shrinking.
“We suspect this growing relative inexperience is prompting some surgeons to sometimes undertake complicated endovascular solutions for problems that could be repaired in a much more straightforward manner using open surgery,” says Dr. Caputo. He notes that he and his colleagues see evidence of this on a consistent basis.
Consider the below CTs from a 55-year-old man who had undergone an aorto-uni-iliac configuration for EVAR along with a femoral-femoral bypass and three coilings.
Advertisement
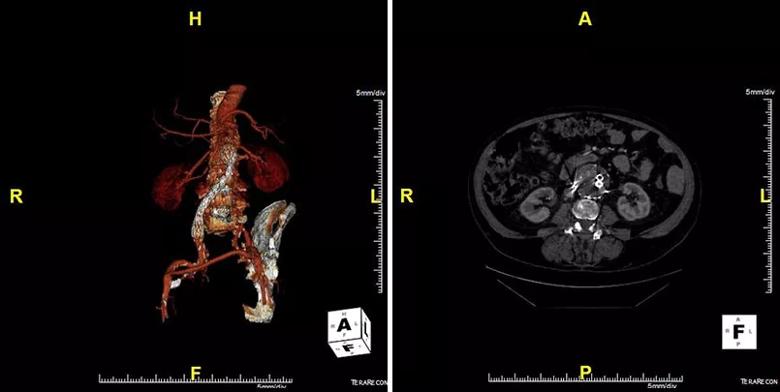
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a2d1d82d-e01a-467a-81ed-cc80a2fb3203/18-HRT-5576-failed-EVAR_Inset-4_jpg)
When the patient encountered difficulties and required aortic endograft explant at Cleveland Clinic, the complexity of the material removed was striking, resembling a tackle box, as shown in the photo on the left below. The photo on the right shows the ostia of his right and left renal arteries and of his superior mesenteric artery. “Fortunately, only the intima came out, not the adventitia,” Dr. Caputo observes.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4909f72a-dd1e-41a8-8443-92f9a275406c/18-HRT-5576-failed-EVAR_Inset-5_jpg)
In the context of diminishing experience with open aortic surgeries, cases like this remind Drs. Caputo and Lyden of Occam’s razor — i.e., that simpler solutions are likely to be better than complex ones. While EVAR remains a valuable minimally invasive option for many patients, they point out, abdominal aortic aneurysms are not suited to one-size-fits-all solutions. “Some patients are still best served by a good old-fashioned open repair,” Dr. Caputo concludes.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more