New combination overcomes resistance
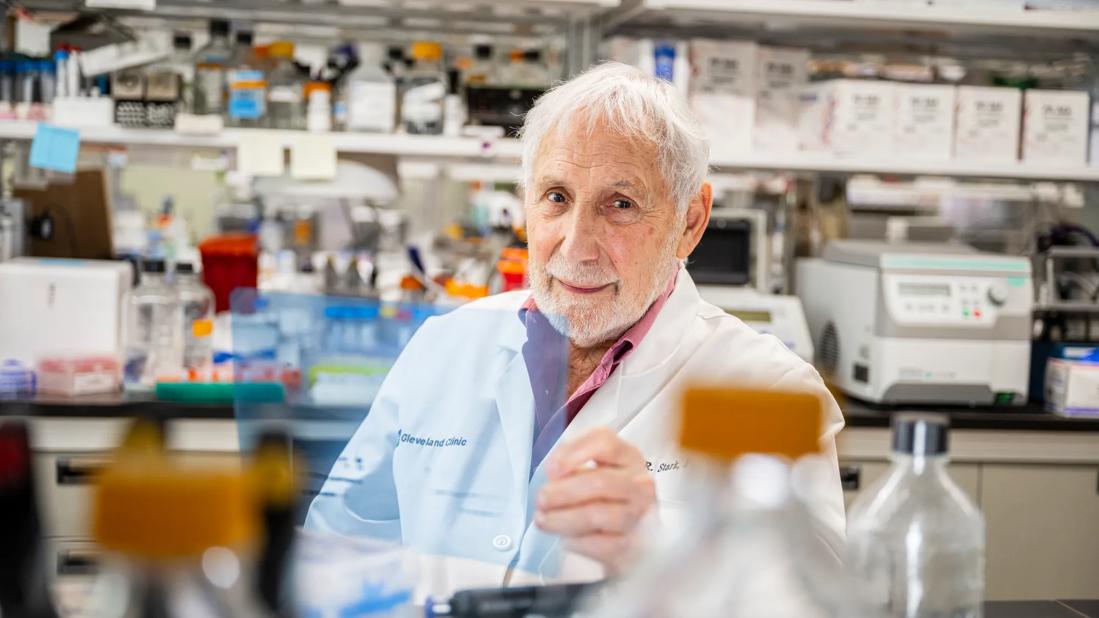
New research from the laboratory of George Stark, PhD, Lerner Research Institute Department of Cancer Biology, suggests that combining cisplatin with a new experimental drug called CBL0137 is highly effective in treating small cell lung cancer (SCLC) and may work by affecting three different pathways.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
CBL0137 — which was discovered at Cleveland Clinic in the laboratory of Andrei Gudkov, PhD, DSci, former chair of Lerner Research Institute’s Department of Molecular Biology (now renamed) — has been shown to have positive effects in several types of cancer. To investigate the drug’s potential efficacy in SCLC, the researchers treated four SCLC cell lines—three patient-derived and one derived from a preclinical disease model—with either cisplatin, CBL0137 or a combination of both drugs. The combination therapy greatly reduced tumor growth compared with the cells treated with either drug alone, suggesting that CBL0137 helps prevent and overcome cisplatin resistance.
Further analysis revealed that CBL0137’s potency in SCLC is multidimensional. The study findings suggest that CBL0137 attacks a combination of three different cellular pathways that contribute to chemotherapy resistance.
Cisplatin damages sections of DNA that encode various pro-cancer pathways, leading to cancer cell death or cycle arrest. SCLC cells eventually learn to self-repair these damaged sections of genetic code, enabling them to evade the drug’s effect in the future. A protein analysis showed that CBL0137 inhibits the activity of the histone chaperone protein called FACT (facilitates chromatin transcription), which plays an important role in this DNA repair process. This is one way CBL0137 may help prevent resistance.
FACT also contributes to cancer by regulating the expression and function of several stem cell transcription factors (SOX2, Nanog, Oct4), which enable the cells to self-renew. A subset of SCLC cells called tumor-initiating cells (TICs) abundantly express these proteins, can self-renew and, therefore, are believed to contribute to cisplatin resistance. In both TICs and non-TICs, CBL0137 treatment reduced expression of these dangerous proteins and cancer cell survival, but a significantly greater effect was observed in TICs. This suggests that CBL0137 preferentially targets the pro-cancer FACT pathway in TICs. Since SCLC tumors have higher levels of TICs than non-TICs, this is another way CBL0137 may work to fight cisplatin resistance.
Advertisement
Lastly, Dr. Stark and colleagues found that CBL0137 activates an important tumor-suppressing gene that is normally turned off in TICs. NOTCH, a gene which has been implicated as a major player in several types of cancer, is expressed more abundantly in non-TICs than TICs suggesting it helps prevent tumors. Through a series of protein binding analyses, the researchers discovered that in SCLC cells, an inhibitory protein, called SP3, binds to the NOTCH promoter and silences the NOTCH signaling pathway, which allows tumors to grow and spread unchecked. CBL0137 prevented this binding, which allowed the anti-cancer NOTCH pathway to stay activated.
Taken together, these findings offer great hope that supplementing chemotherapy treatment with CBL0137 may prevent cisplatin resistance and effectively treat SCLC. Understanding the cellular mechanisms at play will be very important for future studies, which are already moving forward. Dr. Stark’s laboratory has received a grant from the Department of Defense to continue this work in other cell culture and preclinical models.
“We are optimistic that the important findings from this study bring us ever closer to a clinical trial to test the efficacy of this combination therapy in humans,” said Dr. Stark. “We want to bring this basic discovery to the patient bedside as quickly as possible, to help improve the currently poor outcomes for those patients who are diagnosed and live with SCLC.”
This first phase of study was funded by VeloSano, Cleveland Clinic’s flagship campaign to raise money for cancer research. In four years, the initiative has raised more than $12 million.
Advertisement
Dr. Stark is a Distinguished Professor of the Lerner Research Institute and former institute chair. He is a pioneer in the field of cancer biology and a member of the National Academy of Sciences and fellow of the Royal Society of London.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology