The rare disease, which currently has no established treatment, is associated with significant morbidity
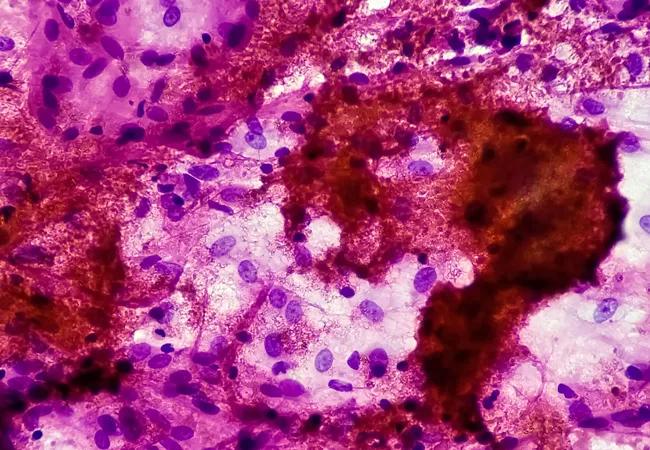
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d8cc0091-39d0-4f42-82b9-0905c46c1949/22-PUL-2762508-CQD-_-Fibrosing-Mediastinitis-and-our-new-center-Francisco-Almeida_jpg)
Histoplasmosis
Fibrosing mediastinitis (FM) is a rare condition that may develop as a consequence of another disorder, usually infection or inflammation. The most common cause in the U.S. is believed to be due to an endemic fungal infection, histoplasmosis, which is very common in Ohio, Missouri and Mississippi River Valley regions. The condition is characterized by mediastinal lymph node enlargement and eventually leads to an intense immune reaction. The lymphadenopathy and conglomerate mediastinal tissue may get calcified and compress vital structures. Historically there has been no treatment for the condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In order to better understand and better treat FM, Cleveland Clinic created a multidisciplinary center focused on the condition. “Often pulmonologists are puzzled with the condition of FM,” explains Francisco Aécio Almeida, MD, MS, a pulmonologist at the Cleveland Clinic’s Respiratory Institute and one of the leaders spearheading the development of the Center. “That’s the nidus for why we created this center. We want to improve the management of patients with FM and provide them with potential options. The latter would include innovative medical therapies, endobronchial or intravascular procedures and the latest surgical interventions. The center will also provide a platform for education and research.”
“Infection with histoplasma can present in many ways,” says Dr. Almeida. “Most of the time it is a mild infection and recognized incidentally as a dormant lung nodule or a calcified lymph node. Occasionally, the calcification can also involve the spleen or the liver.”
In the past, treatment focused on relieving compressions via stent placements in the airway or dilating the esophagus. However, these treatments have potential long-term side effects, especially when airway stents are required. Sometimes surgical procedures are essential to relieve compression of a large vital mediastinal structure. In some instances, part of the lung or the entire lung may need to be removed. For some patients, disease progression may result in the area becoming so scarred that nothing more can be done.
Advertisement
“Eventually the disease gets to a point where there is exuberant scarring of the mediastinum and all efforts remain futile,” says Dr. Almeida. “I have a patient that has such chronic occlusion of a great vessel resulting in the development of collaterals. This response is seen In cases where the mediastinum is so densely fibrotic that any surgical intervention is challenging and a great deal of expertise is required. We take the decision to perform a biopsy or a therapeutic procedure very seriously as the possibility for complications is high.
Dr. Almeida notes that a recent report on FM has indicated that the drug Rituximab could possibly decrease the activity of B lymphocytes and may decrease the inflammation as well as the burden of lymphadenopathy or tissue damage. He explains that although the report was small, the participants showed a great response. The researchers felt that a PET scan may guide the selection of patients who are likely to respond to the therapy. Dr. Almeida says that one of the goals of the center is to further expand on these findings. “We would like to explore the therapeutic value of Rituximab and similar agents,” says Dr. Almeida.
One of the aspects of the Cleveland Clinic’s center that Dr. Almeida is excited about is its multidisciplinary approach. The center will bring together a group of people who have experience and an interest in this condition to brainstorm how they can advance the management of these patients. Our team is made up of pulmonologists, infectious disease specialists, interventional radiologists, cardiologists and pulmonary hypertension specialists. “We’re looking into building the knowledge base so that we can grow together and improve the welfare of these patients.”
Advertisement
Dr. Almeida explains, “We want to centralize the care of patients with FM within the Cleveland Clinic, so we have a group of experts who will see these patients and provide them with the best available comprehensive care.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program