Remotely based physicians use telehealth technology to evaluate lower-acuity patients in the ED, express clinic or during an EMS response

A new Virtual Emergency Medicine Program instituted by Cleveland Clinic in its Northeast Ohio hospitals and medical clinics and in several area emergency medical systems (EMS) is providing expedited care for lower-acuity patients, which helps in managing emergency department (ED) volumes and wait times.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The program uses telehealth technology to connect remotely based emergency medicine physicians with newly arrived and appropriately triaged consenting patients in 13 Cleveland Clinic hospital EDs and 26 Express Care clinics. The remote physicians also can interact with paramedics in four participating EMS services regarding whether to treat low-acuity patients in place or transport to an ED.
After evaluating symptoms, the physicians can order any necessary diagnostic tests, prescribe medications and write follow-up care instructions using Cleveland Clinic’s electronic health record system.
The program frees up ED bed space and enables on-site ED staff and resources to be focused on patients with the most acute needs.
“Having a centralized emergency medicine doctor available around the clock to provide expertise and treat the right patients in a lower-cost, lower-intensity setting is a huge value for our patients and our health system,” says Bruce Graham, DO, of Cleveland Clinic’s Center for Emergency Medicine, who leads the Virtual Emergency Medicine Program. “We’ve replicated the physical ED in the virtual space. Just as EDs get patients from doctor’s offices, EMS and express clinics, we’re doing the same thing virtually.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/882b1c33-a4f7-49da-b506-168adbc1f59c/23-CCC-3954418-Virtual-ED-850x550-1_jpg)
Bruce Graham, DO, who leads Cleveland Clinic’s Virtual Emergency Medicine Program, interacts with a patient.
The program arose from Cleveland Clinic’s desire to leverage technology to make emergency care more accessible and from the healthcare system’s initial experience with a Centers for Medicare and Medicaid Services payment model called Emergency Triage, Treat, and Transport (ET3).
Advertisement
Traditionally, Medicare regulations only allowed payment for emergency ambulance services when patients were transported to hospitals and other acute care facilities. As a result, many patients were treated in hospital EDs, even though a lower-acuity destination may have better suited their needs and incurred lower costs.
In 2019, the federal government unveiled the ET3 model, which expanded options for Medicare patients being transported by ambulance. Under the model, patients needing less serious medical attention could be treated on-scene by an ambulance provider working with a healthcare system via telehealth, or be transported to a lower-acuity facility such as an urgent care center.
“We assisted a couple of local municipalities with getting their EMS accepted into the ET3 model and we were supporting virtual care for them,” Dr. Graham says. “And with a centrally located physician, we could support nursing homes in addition to EMS.
“As we were evaluating the volume and economics of expanding the program, we got hit with COVID,” he says. “We had record numbers of patients coming into our EDs and sometimes we had to station a provider in the lobby to help with triage. Since we already had a remote physician supporting EMS, it became obvious that it would be more effective for that physician to connect virtually to all our Northeast Ohio EDs and provide support when things got busy, rather than having a dedicated in person physician in triage in all of our EDs 24/7. So we evolved to that model.”
Advertisement
Launching the full-scale program required intensive collaboration among representatives of emergency medicine, information technology, virtual health, risk management, legal and regulatory compliance, and revenue cycle. “It took a lot of administrative excellence and time to get to where we are now,” Dr. Graham says.
After 10 months of planning, the Virtual Emergency Medicine Program began in fall 2021 at Cleveland Clinic’s main campus ED and its Avon and Fairview regional hospital EDs. Six months later, the service was expanded to the remaining 10 regional hospitals and physician coverage was extended from 16 hours a day to 24. Efforts to add the service at Cleveland Clinic’s 26 Northeast Ohio Express Care clinics are almost complete.
Although other healthcare systems have implemented emergency medicine telehealth programs, “to my knowledge, no one has done it to our scale,” incorporating multiple hospital EDs, Express Care Clinics, EMS agencies and congregate living facilities, Dr. Graham says. Sixteen Cleveland Clinic physicians, all board certified in emergency medicine, staff the program in rotating shifts.
In the ED triage portion of the program, which accounts for most of the virtual physician/patient interactions, patients who might be candidates for virtual care are identified in one of two ways: By ED intake/triage personnel or by the remote physician who constantly monitors the lobbies of all the EDs by way of EPIC, Cleveland Clinic’s electronic health record.
Low-acuity conditions that qualify for virtual evaluation include upper respiratory infections, sore throats, isolated extremity injuries, rashes, allergic reactions, and minor cuts and burns.
Advertisement
If a patient consents to virtual assessment, they are escorted to a private area separate from the ED clinical space. Physician/patient communication takes place using iPads equipped with customized Microsoft Teams software. The technology is extremely user-friendly; patients only need to touch the tablet screen button to accept the physician’s call.
The waiting time to connect averages less than two minutes, Dr. Graham says.
The physician orders tests, prescriptions and other items using the electronic health record. “Everything that we would do in the emergency department for these types of low-acuity patient, we can now do virtually,” Dr. Graham says.
Patients can view test results and follow-up care instructions with Cleveland Clinic’s MyChart app. The physician can instantly enroll a patient in MyChart if they have not previously used the service.
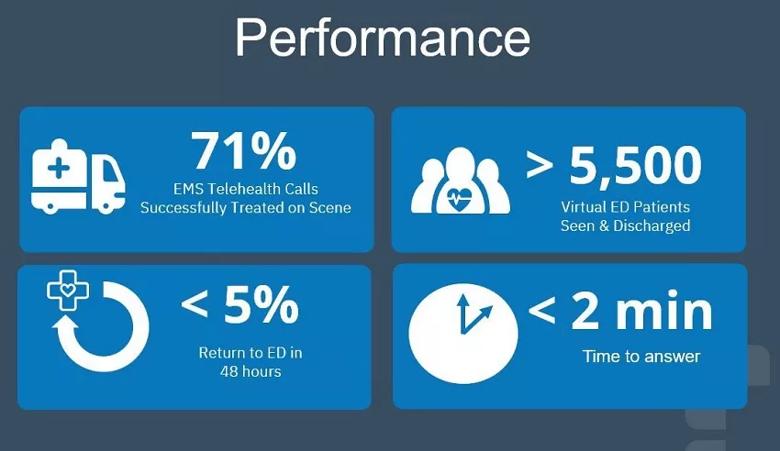
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/48216ad9-8860-494b-8de5-d2febb706015/23-CCC-3954418-Virtual-ED-stat-highlights-850x495-2_jpg)
While the virtual ED program is intended to help manage busy ED waiting rooms, and treat lower-acuity patients on scene, it can function the same way for patients who present with subtle symptoms that require rapid intervention. “We’ve caught neutropenic fevers in cancer patients who are undergoing chemotherapy and have an infection,” Dr. Graham says. “We’ve identified septic patients while they’re still in the ED lobby. There have been a lot of great quality saves that have come out of the program.”
More than 5,500 patients presenting at Cleveland Clinic EDs have assessed virtually and discharged since the program’s start. Less than 5% of those patients have returned to the ED within 48 hours. “That’s a strong indicator that we are safely managing these patients,” Dr. Graham says.
Advertisement
Surveys show 83% of patients are highly satisfied with their virtual interaction. “Patients rave about the experience,” Dr. Graham says. “They’re still getting that one-on-one time with the emergency medicine physician. Our nurses and medics do an excellent job of explaining ahead of time that it’s the same providers that patients otherwise would’ve seen in person in the ED.”
From both a medical and an economic standpoint, every patient who undergoes virtual ED care is one fewer patient who leaves without being treated. “It’s good for the patient, it helps us improve resource management and it’s also capturing fee-for-service revenue that otherwise would have been lost,” Dr. Graham says.
The Virtual Emergency Medicine Program also ensures that patients receive care in the most cost-effective setting, which benefits patients and insurance providers. Seventy-one percent of patients assessed virtually during an EMS-initiated telehealth call with the Cleveland Clinic program were treated on scene, without need for transport to the ED.
With the program’s success in Northeast Ohio, Dr. Graham says there may be opportunities for further expansion, including at Cleveland Clinic facilities in Florida.
Advertisement

This technical solution expedites the patient’s ED to admissions process

Akron General and Union Hospital increase throughput and patient satisfaction by rethinking their approach to care

Peer-to-peer videos offer creative solution to help patients while they wait

Advanced connectivity and technologies build on a foundation of teleneurology leadership

Remote caregivers allow bedside nurses to breathe easier when out of a patient’s room

Phone triage system reduces call backs and delays in care

Caregiver collaboration and patient education remain critical

Mode of delivery does not affect patient satisfaction