Insights on leveraging collaboration and advocacy to develop and conduct needed trials
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/13534509)
Developing successful clinical trials for rare conditions, such as brain tumors and spine tumors, is challenging. But the potential to help patients drives neuro-oncologists like Mark Malkin, MD, of Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“There are a number of challenges to the development of clinical trials,” says Dr. Malkin. “Ultimately, we hope to translate genetic discoveries from the Human Cancer Genome Project and the Cancer Genome Atlas into therapeutic options for patients and personalize the options, which may differ from one patient to another.”
In the most recent episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Malkin discusses challenges and opportunities in clinical trials for brain and spine tumors and how they influence study design. He delves into:
Click the podcast player above to listen to the 30-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
This activity has been approved for AMA PRA Category 1 Credit™. After listening to the podcast, you can claim your credit here.
Podcast host Glen Stevens, DO, PhD: You’ve talked about some of the difficulties with the treatment of these tumors. Where do we go from here?
Dr. Malkin: We start with collaboration. Lots of smart people with what appear to be brilliant ideas haven’t yet been able to crack this nut working individually. So we need to build teams of teams. Within our institutions we need clinicians to be taking problems from the bedside to the bench — to our lab science colleagues — and then bring back something we can test in clinic.
Advertisement
We need to also involve and take advantage of the discoveries of our colleagues with expertise in molecular pathology and mutations, as well as the huge advances in imaging and big data and artificial intelligence. Phil Gutin, who was chair of neurosurgery at Memorial Sloan Kettering Cancer Center when I was practicing there, said almost 15 years ago that neurosurgery would become a specialty that puts things into the brain rather than just taking things out of the brain. We are getting to that point now.
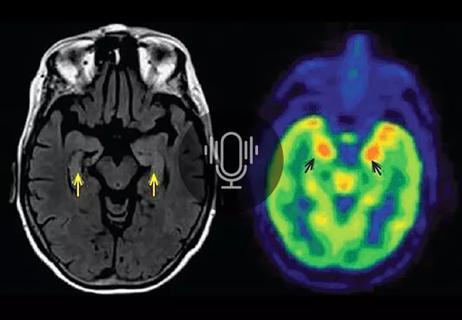
We are also getting to the point, with advanced imaging and artificial intelligence, where we can tell on an MRI scan whether a tumor is IDH [isocitrate dehydrogenase] wild-type or IDH mutated. That’s important because the IDH mutated tumors tend to have a better prognosis. Being able to diagnose without a biopsy is very cool, and presumably one can follow response to therapy without a biopsy. One needs supercomputers and big data to look at the genome of an individual tumor to try to pick out which mutations might be driver mutations — what we call trunk mutations — from all the other background noise. That will help focus the laboratory effort on important mutations and avoid distraction by issues of secondary importance.
We also need more advocacy for patients with brain tumors. We need advocacy on the level at which the breast cancer community has advocacy. They have figured this out really well with the Susan G. Komen Foundation. It helps that the tragic circumstances that surround the Biden family, in terms of the death of Beau Biden, are leveraged by someone who is now President and in a position to move things forward like the Cancer Moonshot initiative. More advocacy means more visibility and ultimately more funding.
Advertisement
Advertisement

New research focuses on tumorigenic aspects of communication among brain cells
Evidence hints that chronic neuroinflammation might stem from a CNS-directed autoimmune response

Research shows promise for use in therapeutic settings to manage depression, PTSD, anxiety and more
Comprehensive evaluation and keen clinical judgment are key in suspected cases

Why we’ve launched a targeted mentorship program and new dedicated funding awards

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Planning continues with critical, patient-focused input from nursing teams

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood