Case series finds simultaneous repair to be safe, feasible and often advantageous
Pectus excavatum repair using a modified Ravitch technique can safely be combined with cardiac surgery in a single operation, with low bleeding risk and good long-term outcomes. That’s the conclusion of the authors of a series of 11 patients who underwent the complex surgery at Cleveland Clinic as reported in Seminars in Thoracic and Cardiovascular Surgery (2021 Mar 6; online ahead of print).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We published our experience to let surgeons know that combining pectus repair with cardiac surgery is a viable option for patients with multiple indications for the operation,” says Cleveland Clinic thoracic surgeon Daniel P. Raymond, MD, senior author of the case series. “We also want to increase awareness that pectus excavatum has implications beyond cosmesis.”
Especially in patients with a connective tissue disorder, pectus excavatum and congenital or acquired heart disease are often found together. Whether a staged or combined strategy is best to address both problems has not been well established, and few reports of simultaneous repair exist in the literature.
Those who argue for a staged approach cite bleeding, sternal wound infections, complicated sternal reentry (if required) and chest wall instability as potential complications of a single procedure. On the other hand, simultaneous repair offers the opportunity to correct cardiac problems and relieve the compression of cardiac chambers and restrictive lung disease brought about by severe pectus excavatum in a single operation.
“Pectus excavatum can be an important source of pathology by causing distortions in cardiac anatomy,” says Cleveland Clinic cardiac surgeon Patrick Vargo, MD, a co-author of the case series. “Compression by the chest wall can make it difficult to determine the cause of symptoms, contribute to cardiac dysfunction and make surgical outcomes less predictable if left untreated.”
The series consisted of patients who underwent a modified Ravitch procedure for severe pectus excavatum at the time of cardiac surgery at Cleveland Clinic between 2012 and 2020.
Advertisement
There were 11 patients with the following characteristics:
The patients’ concomitant cardiac procedures were valve-preserving aortic root replacement (n = 7) or mitral valve repair (n = 4). Surgical details and outcomes were as follows:
There were no reoperations for bleeding, tamponade or other indications, and no deaths occurred in-hospital or during follow-up.
Dr. Raymond emphasizes the importance of a multidisciplinary team when considering performing this combined surgery. He notes that pectus excavatum is rare enough that most cardiac surgeons do not have the experience to contemplate conducting both operations at once. He adds that patients managed by Cleveland Clinic’s Center for Chest Wall Disease are evaluated by cardiac surgery, cardiology and cardiothoracic anesthesiology teams preoperatively.
Drs. Raymond and Vargo highlight the following critical points from their experience:
Advertisement
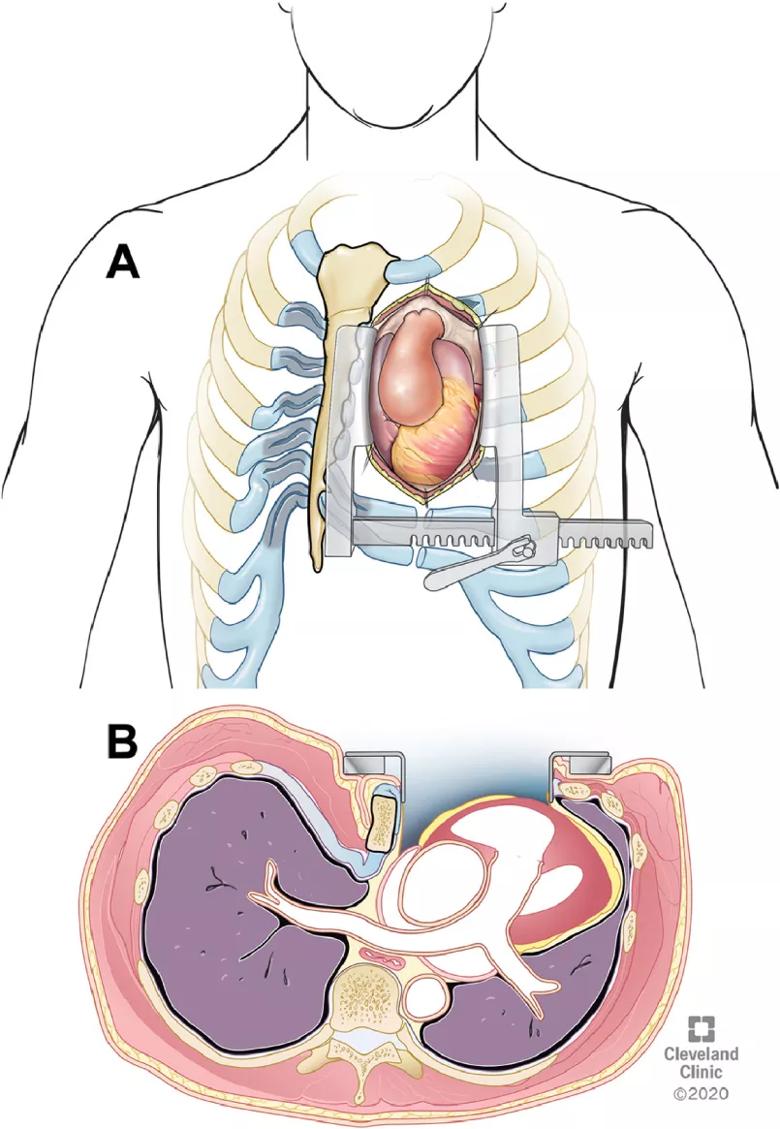
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b95f54e2-c925-4ffe-827c-8da08ddd3e59/21-HVI-2215858-inset-pectus-excavatum-repair-805x1165-1_jpg)
Figure. (A) A Cooley sternal retractor is placed to visualize the mediastinum. As the retractor is opened, the sternum is rotated and retracted to the right for optimal exposure of the heart and aortic root aneurysm. (B) Axial illustration of the rotation and retraction of the sternum with the retractor opened. Reprinted from Zaki et al. Semin Thoracic Cardiovasc Surg (2021 Mar 6; online ahead of print). © 2020 The Cleveland Clinic Foundation.
Advertisement
In a commentary accompanying the article, two thoracic surgeons from Brigham and Women’s Hospital and Harvard Medical School wrote: “The addition of a Ravitch to open cardiac procedure, besides being ideal in the synchronous management of two pathologies that impact one another, allows the patient to recover from one procedure. When done with skill and expertise, the outcomes can be superb.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more