Management is guided by patient and tumor characteristics, institutional expertise
If esophageal adenocarcinoma is diagnosed early — when isolated to the mucosal and submucosal layers of the esophagus — it carries a favorable prognosis. Treatment of early esophageal cancer has focused primarily on resection — either surgical or, more recently, endoscopic. Radiation therapy and chemotherapy have historically been considered in patients in whom the cancer is more advanced. In virtually all cases, a multidisciplinary approach may help identify the best therapeutic strategy based on patient and tumor characteristics and local expertise.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The components of such an approach are the focus of a recent review in the Cleveland Clinic Journal of Medicine (2022;89[5]:269-279) by a multidisciplinary team of Cleveland Clinic clinicians. This article summarizes key points from the article relating specifically to treatment of early esophageal adenocarcinoma — from cancer staging to surgical and endoscopic resection, chemoradiation, adjuvant therapy and surveillance following curative endoscopic resection. The Cleveland Clinic team’s suggested care path for early esophageal adenocarcinoma is summarized in the figure below.
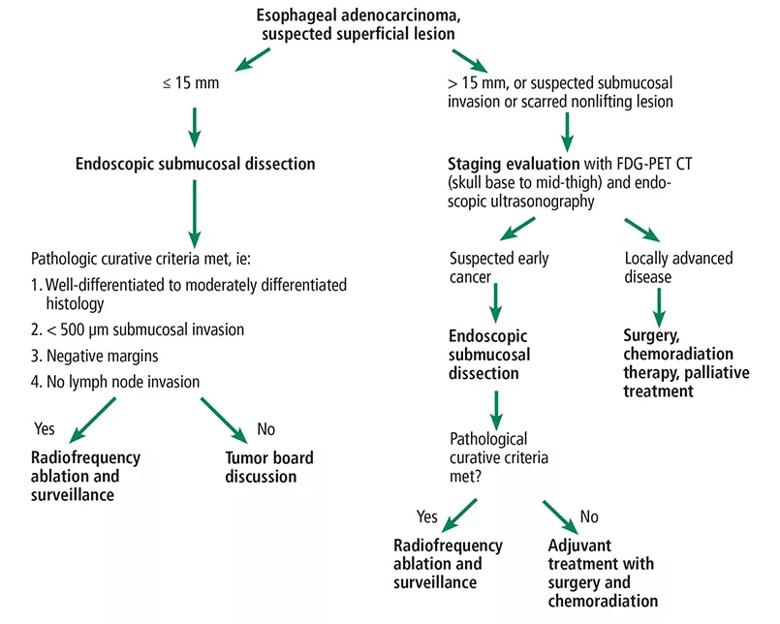
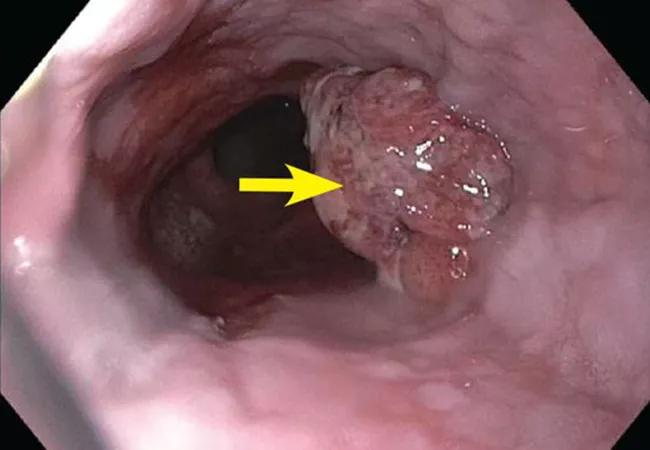
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/063b5528-5053-4641-b8ce-9fb3f06750d1/22-HVI-3042609-CQD-Inset1_jpg)
Figure. The Cleveland Clinic care path for early esophageal adenocarcinoma.
Once esophageal adenocarcinoma is diagnosed, its stage needs to be assessed to determine prognosis and treatment. This involves the tumor, lymph node status and metastasis (TNM) staging system based on tumor depth (from T0 to T4), number of affected lymph nodes (from N0 to N3) and metastasis to distant organs (M0 [absent] or M1 [present]).
The role of PET/CT imaging and endoscopic ultrasonography in early esophageal adenocarcinoma staging is controversial. However, guidelines from the National Comprehensive Cancer Network recommend staging by PET/CT and endoscopic ultrasonography in cases of advanced cancer (≥ T1b) to evaluate for nodal spread. PET/CT is less beneficial in early esophageal adenocarcinoma than in advanced disease. In their review, the Cleveland Clinic authors write that they consider PET/CT before resecting bulky or borderline tumors larger than 15 mm or lesions with suspected superficial submucosal invasion greater than 500 μm.
Advertisement
Endoscopic ultrasonography can assess for the depth of tumor invasion and locoregional lymph node spread. However, it has a high false-positive rate (up to 10%) for nodal disease detection. As a result, guidelines from the American Society for Gastrointestinal Endoscopy strongly recommend against its routine use in early esophageal adenocarcinoma to stage mucosal (T1a) and submucosal (T1b) disease for determining nodal status.
“In recent years, more advanced tumors are being referred for endoscopic resection,” observes review co-author Siva Raja, MD, PhD, Surgical Director of the Center for Esophageal Diseases in Cleveland Clinic’s Department of Thoracic and Cardiovascular Surgery. “For this reason, accurate staging and ruling out advanced disease before proceeding with endoscopic treatment is paramount. Further research is needed to understand the role of PET/CT and endoscopic ultrasonography in large T1a (> 15 mm) and early T1b disease that is increasingly being referred for endoscopic resection.”
For decades, first-line treatment for early esophageal adenocarcinoma, including Barrett esophagus (a pre-cancerous lesion), has been open surgical resection. Technical advances in surgery such as robot-assisted minimally invasive esophagectomy, minimally invasive esophagectomy and 3D imaging have improved recovery times and lymph node yield and significantly reduced postoperative pain, intraoperative bleeding and hospital length of stay.
In recent years, minimally invasive surgical approaches have become preferred, with long-term results that are not inferior to those of open esophagectomy but with less morbidity.
Advertisement
The role of surgical esophagectomy remains controversial in early T1a tumors with high-risk features such as poor differentiation and large size, due to higher rates of perioperative mortality and morbidity with potentially a similar risk of locoregional spread. However, T1b tumors in otherwise healthy patients are considered for immediate esophagectomy due to the established higher risk of lymph node metastasis.
Postoperative complications affect long-term mortality rates. Procedure-specific complications include conduit abnormalities and recurrent laryngeal nerve injury; systemic complications include atrial fibrillation, myocardial infarction and pneumonia. Long-term sequelae of esophagectomy include functional disorders such as dysphagia, delayed gastric emptying, reflux and dumping syndrome. However, esophagectomy is usually well tolerated long-term with lifestyle changes such as eating frequent small-portion meals slowly and avoiding high-sugar foods and beverages.
Modern endoscopic techniques and devices have led to a shift toward endoscopic treatment of early esophageal cancer rather than surgery, although not all early esophageal adenocarcinomas are amenable to curative endoscopic resection.
Endoscopic resection can be considered in tumors at low risk for lymph node metastasis or in higher-risk tumors in patients who are medically unfit for surgery. “The risks of perioperative death and of regional spread can be between 3% and 4%,” notes Dr. Raja. “Therefore, it is important to weigh the risk of lymph node metastasis and the risk of morbidity and mortality of surgery in a patient before deciding the best therapeutic approach for early esophageal adenocarcinoma.”
Advertisement
There are two main endoscopic resection techniques: (1) endoscopic mucosal resection and (2) endoscopic submucosal dissection. The safety, success rates and procedural ease of endoscopic mucosal resection have established it as a mainstay in the treatment of early esophageal adenocarcinoma. However, for larger lesions, endoscopic mucosal resection requires removing the tumor in multiple pieces, which is associated with higher recurrence rates. In contrast, endoscopic submucosal dissection can allow removal of even larger tumors in a single piece (en bloc) and is associated with higher rates of cure and a lower risk of recurrence; it also allows for precise histopathologic analysis.
Early esophageal adenocarcinoma is primarily managed with endoscopic resection (T1a) or surgery (T1b). However, emerging data hint at a role for neoadjuvant (before resection) or adjuvant (after resection) chemoradiation therapy in early disease, particularly in patients with high-risk tumors (incomplete resection, positive deep margins, lymphovascular invasion, poorly differentiated tumors, tumors larger than 2 cm) who are medically unfit for surgery with lymph node dissection.
Paclitaxel and carboplatin are commonly used with concurrent radiotherapy. Another combination increasingly being used is 5-fluorouracil and oxaliplatin concurrent with radiotherapy. An ongoing randomized trial is comparing these two adjuvant regimens for resectable esophageal adenocarcinoma.
Radiotherapy alone (external-beam or brachytherapy) can be an option for patients over age 65 with esophageal adenocarcinoma who cannot undergo surgery or endoscopic therapy and concurrent chemotherapy. Poor surgical candidates who are definitively treated with chemoradiation can have residual, recurrent or metachronous disease. These patients can be managed selectively with salvage endoscopic submucosal dissection or ablation therapy.
Advertisement
Further study is needed to explore the utility of neoadjuvant or adjuvant chemoradiation in early esophageal adenocarcinoma, the review authors note.
Patients with early esophageal adenocarcinoma are increasingly being treated with endoscopic resection. However, some resections are noncurative, with poor differentiation, lymphovascular invasion, deep submucosal invasion or positive margins. These patients are at higher risk of lymph node metastasis and progressive disease.
Ideally, esophagectomy with or without adjuvant chemoradiation therapy is the treatment of choice for these patients. However, patients who have high-risk features after endoscopic resection and are poor surgical candidates for definite esophagectomy with lymph node dissection can be referred for chemoradiation therapy.
In esophageal adenocarcinoma, endoscopic resection is considered curative if the resection histology is well to moderately differentiated with no lymph node invasion and with less than 500 μm submucosal invasion combined with negative lateral and deep margins, according to European Society of Gastrointestinal Endoscopy guidelines.
Patients who undergo complete endoscopic resection of Barrett esophagus or esophageal adenocarcinoma are enrolled in a posttreatment surveillance program. Posttreatment surveillance is stratified based on postresection pathologic staging, as follows:
Early esophageal adenocarcinoma is often diagnosed serendipitously in patients without symptoms undergoing upper endoscopy for other reasons. Due to the unique anatomy of the esophagus, even early esophageal adenocarcinoma has a risk of lymph node metastasis, and appropriate management is necessary.
For small esophageal adenocarcinoma lesions (i.e., < 1.5 cm), multiple studies have shown endoscopic mucosal resection to be an effective strategy with good long-term results. For larger lesions or suspected deeper invasion or squamous cell carcinoma, a multidisciplinary approach is warranted. Endoscopic submucosal dissection can be effectively used to remove superficial tumors, despite their size or associated fibrosis. However, for lesions involving more than two-thirds of the circumference of the esophagus, there is a risk of esophageal stricture formation.
“Patients with early esophageal adenocarcinoma and risk of lymph node metastasis are best treated with surgical resection, which allows for lymph node dissection, but many patients over age 65 or with significant comorbidities may not be candidates for surgery,” says review co-author Sudish Murthy, MD, PhD, Section Head of Thoracic Surgery at Cleveland Clinic. “In these patients, endoscopic resection with adjuvant chemotherapy or radiotherapy can be considered.”
The review concludes by noting that some patients with early esophageal adenocarcinoma may not be candidates for either endoscopic or surgical resection, owing to severe comorbidities. In these patients, radiotherapy, brachytherapy, chemotherapy or a combination of these can be performed.
The full-length Cleveland Clinic Journal of Medicine review is freely available here.
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more