Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Risk of lung cancer spread through air spaces (STAS) is increased in younger patients with clinical T1-3N0 M0 disease, solid tumors ≥ 2 cm, KRAS mutations and high uptake on positron emission tomography (PET) scans. So reveals a retrospective Cleveland Clinic study of preoperative predictors of STAS in non-small cell lung cancer (NSCLC). The findings were published in the Journal of Thoracic and Cardiovascular Surgery (Nov 23:S0022-5223(23)01106-6).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our study identifies preoperative characteristics that are predictive of STAS,” says Cleveland Clinic thoracic surgeon Monisha Sudarshan, MD, MPH, the study’s principal investigator. “The results can be used to guide decisions about whether to perform sub-lobar resections or more extensive surgery.”
STAS is associated with higher rates of NSCLC recurrence and lower rates of survival, particularly in patients who undergo limited resection, but it can’t be used intraoperatively because of low sensitivity and specificity on frozen sections. As a result, final pathology from supposed “definitive” segmentectomies or wedges sometimes indicates STAS, creating a treatment conundrum for surgeons.
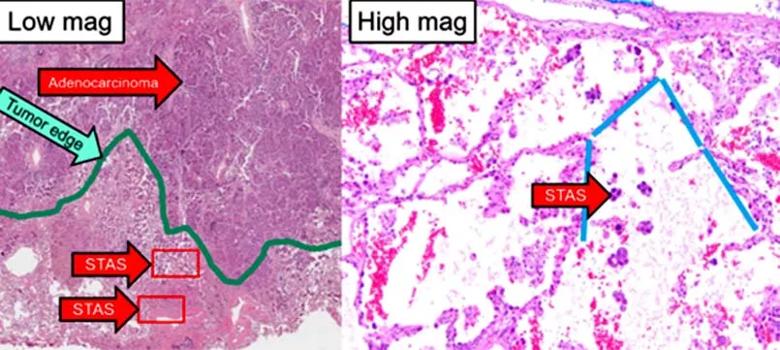
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9ec74648-804b-4c5c-898a-719fd716b3ba/histology-showing-stas)
Pathological findings of spread through air spaces (STAS). Images courtesy of Sanjay Mukhopadhyay, MD, Cleveland Clinic.
To help address that situation, the researchers analyzed data from 439 patients with clinical T1-3N0 M0 NSCLC who underwent primary surgery at Cleveland Clinic between January 2018 and December 2021. The majority were women (58%) and ever-smokers (83%) who had been diagnosed with adenocarcinoma (90%) and had undergone lobectomy (84%).
Preoperative markers evaluated were age, sex, smoking status, tumor size, ground-glass opacities, maximum standardized uptake value (max SUV) on PET, and molecular markers on preoperative biopsy. Standardized mean differences were used for between-group comparisons and random forest classification for prediction modeling.
“We have used nonlinear, nonparametric machine learning to analyze preoperative predictors of STAS which is not common in the literature,” notes first author Sadia Tasnim, MD, a Cleveland Clinic thoracic surgery fellow. “This approach facilitated straightforward interpretation of confounders and is superior to multivariable logistic regression for predicting events.”
Advertisement
At least one STAS-positive tumor was found in 177 of the patients; the remaining 262 patients had no STAS-positive tumors. Overall, 179 STAS-positive tumors and 293 non-STAS-positive tumors were evaluated.
Age ͏≤ 50 years, solid tumor, size ≥ 2 cm and max SUV ≥ 2.5 all were independently predictive of STAS, with probabilities of 50%, 40%, 38% and 40%, respectively. STAS tumors also were more likely to harbor KRAS mutations and to be PD-L1 negative. Non-STAS tumors, in contrast, were more likely to express PD-L1. Gender, body mass index, race and smoking status were not linked with predisposition to STAS.
“We hypothesized that STAS would be more likely in older patients, based on previous reports in the literature, but our study showed the opposite,” Dr. Sudarshan notes. “We don’t know why that is the case, and we hope to do a study of STAS in younger patients to help answer this question.”
Of the 42 patients who had a recurrence of cancer, 19 were in the STAS group and 23 in the non-STAS group. However, no difference between the groups was noted for freedom from recurrence.
While the factors identified by the authors are individually predictive of STAS, taken together, they may have an even more powerful effect on treatment. The study report considers the potential clinical ramifications in two hypothetical cases, both involving NSCLC that measures 2 cm:
Advertisement
“Based on our findings,” Dr. Tasnim says, “patient 1 has a cumulative predicted probability of STAS of 60%, and a lobectomy would be warranted if preoperative cardiopulmonary characteristics permit. A limited resection is appropriate for patient 2 because their cumulative predicted probability of STAS is only 20%.”
The authors note that considering more rather than less extensive surgery in younger individuals runs counter to current thinking about what constitutes definitive therapy for this population. They also acknowledge that high-quality data from randomized clinical trials are needed to justify a completion lobectomy.
For now, they hope their data will lead to “lightbulb” moments for thoracic surgeons when they have patients with features predictive of STAS and will prompt consideration of a procedure other than sub-lobar resection in these cases.
“Future studies are needed to determine the role of completion lobectomy versus observation or segmentectomy versus lobectomy for patients with STAS,” Dr. Sudarshan concludes. “The role of driver mutations in predicting STAS and their pathophysiology also should be explored to elucidate the natural history and guide targeted therapy for STAS.”
Advertisement
Advertisement
Treatment assigned FDA review date in June 2025
Cleveland Clinic, the University of Minnesota and University of Cambridge receive $1M grant to develop point-of-care biosensor for early detection and treatment personalization
Hybrid treatment model helps improve cancer care access
Resection, radiotherapy or ablation?
Extent of baseline burden impacts progression-free and overall survival
Quantum computing being studied as a means to help improve predictive performance, accuracy
Targeting DNMT1 shows promise in chemotherapy- and immunotherapy-resistant SCLC
New review published in Cancers suggests a synergistic benefit