Findings from a 2023 ASCRS presentation indicate that both 2-stage and modified 2-stage approaches are viable management strategies for Crohn’s patients who require a temporary ileostomy
For patients with high-risk ilecolic Crohn’s disease (CD) who have malnutrition, penetrating disease, steroid therapy or need emergency surgery, a better understanding of optimal management strategies is needed. A recent presentation at the 2023 American Society of Colon and Rectal Surgeons (ASCRS) Annual Meeting compared a traditional 2-stage approach with ileocolic anastomosis and diverting loop ileostomy (ICA-DLI) with a modified 2-stage ileocolic resection (ICR) with end ileostomy (ICR-EI) to determine if one should be favored when trying to reduce complications in patients who received an ileostomy at the time of ICR.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This research came out of a previous study that we presented at ASCRS a couple of years ago which focused on high-risk ileocolic Crohn’s disease,” explains Stefan Holubar, MD, MS, Section Chief of the Inflammatory Bowel Disease Section and Director of Research for the Department of Colon & Rectal Surgery at the Digestive Disease & Surgery Institute and corresponding author on the study. “We looked at patients who had ileocolic anastomosis with and without a diverting loop ileostomy, but in that study, we left out the patients who had an end ileostomy.”
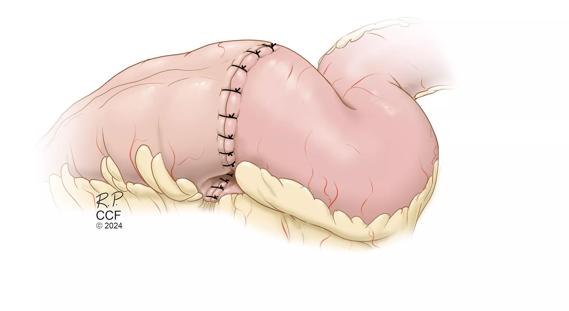
He continues, “In this follow-up study, we wanted to compare patients who all had staged surgery and who were high risk for complications. We compared patients who had an ileocolic anastomosis with a diverting loop ileostomy as their first operation followed by a loop ileostomy reversal with those who had an ileocolic resection with an end ileostomy as the first operation, and that the second operation they got reanastomosis without a loop ileostomy.”
The group queried the prospective inflammatory bowel disease (IBD) registry at Cleveland Clinic with chart review for patients with CD who underwent ICR with loop or end-ileostomy from 1997-2022. Patients who did not or had not yet undergone reversal, or who had 3-stage operations (n = 34) were excluded from the study. The group reviewed perioperative variables and 30-day outcomes for both index resection and subsequent ileostomy. Univariate analyses were performed to compare 2-stage and modified 2-stage approaches. Anastomotic leaks (AL) were defined as an anastomotic fluid collection observed on cross-sectional imaging that included signs of sepsis or radiographic contrast extravasation. The primary outcome of the study was the overall AL rate, and the secondary outcome was the overall complication rate.
Advertisement
Over the 25 years included in the study, 326 patients underwent either 2-stage (n = 268, 82.2%) or modified 2-stage (n = 58, 17.8%). The median age of the patients was 35.4 years. At the initial ICR, the 2-stage and modified 2-stage groups had similar (p > 0.05) characteristics. Steroid rates were 50.7% for the 2-stage group and 29.3% for the modified 2-stage group; weight loss (16.7% vs. 10.3%, respectively), penetrating disease (41.7% vs. 24.1%), immunomodulators (20.8% vs. 13.7%) and biologics (36.9% vs. 17.2%). Dr. Holubar also notes that the modified group had triple the rate of emergent/urgent operations (5.2% 17.2%, p < 0.01).
After the initial ICR, both the 2-stage and modified 2-stage groups had similar rates of readmission (19% vs 24.1%, p = 0.37, respectively) and reoperation (2.9% vs 3.4%, p = 0.85). The median times for ileostomy closures was 19.4 ± 25.6 vs 22.4 ± 12.8 weeks. In the 2-stage group, the initial ICA AL rate was 1.8%, and in the DLI-R, the AL rate was 0.3% for a total of 2.1%. In the modified 2-stage group, there were no instances of ICA leak. The overall 30-day complication rate for the 2-stage and modified 2-stage groups was 58.9% vs 60.3%, p = 0.84, respectively. The modified 2-stage group had a longer total length of stay in the hospital (10.5 [8.0, 14.0] vs 14.0 [10.0, 17.2], p < 0.01 days).
“We found that, overall, patients from both groups did quite similarly,” says Dr. Holubar. “However, patients who had the modified two-stage had a longer total length of stay, which isn’t that surprising since those were typically emergency cases. With this study in particular, surgeon discretion played a major role, and the modified two-stage patients were typically the ones that the surgeons were most worried about leaks. For these high-risk patients who have emergency presentations, hypoalbuminemia, weight loss, penetrating disease, anemia, on corticosteroids, etc., our study indicates that the modified two-stage may avoid some anastomotic leaks in both the short- and long-term.
Advertisement
Dr. Holubar notes that in his study from a couple of years ago, the group calculated the number of risk factors and found that when a patient had greater than three risk factors, the leak rate was over 5%. But as more risk factors were added, the leak rate could be up as high as 17%. “In the present study, we would expect these high-risk patients to have higher leak rates,” he explains. “But those patients who didn’t have anastomosis didn’t have an opportunity to leak at the first operation.
He continues, “There’s an adage, ‘The anastomosis that is not made will not leak.’ The interesting thing was that, when these patients got healthy and were taken back for their end-ileostomy closure and restoration of intestinal continuity, we did not observe any leaks in that group. But it was only 55 patients, so we may have been underpowered.”
Dr. Holubar also notes that one important consideration is the ease of reversing the end ileostomy. While a loop ileostomy can be reversed with a small incision and a success rate of about 90% to 95%, the local incisional reversal for the modified two-stage approach can be harder. Success rates were about 75%, “the main reason they could be reversed locally was adhesions, but I’d take a larger incision over a leak any day.”
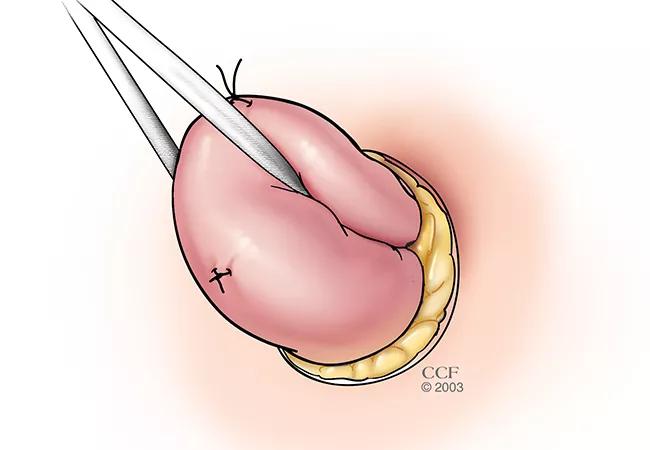
“One nuance of the modified two-stage approach is that we do a subcutaneous implantation of the colonic stump above the fascia so that we know exactly where it is to facilitate reversal,” Dr. Holubar explains. “We like to think a couple of steps ahead in our department. By implanting that colonic stump, you’re avoiding two things. You’re avoiding that stump leaking intra-abdominally, and you’re also facilitating ease of reversal at the second operation.”
Advertisement
Advertisement

Study utilizes prospective data from the RISK cohort

Nationwide research underscores the importance of individualized treatment
Findings support the safety of the technique

Strong patient communication can help clinicians choose the best treatment option

New research identifies a direct functional link between creeping fat and muscle

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Findings help close the knowledge gap around VTE practice patterns