Experienced team makes complex redo possible
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Our patient is a 62-year-old male with severe secondary sclerosing cholangitis following a complex history of biliary reconstruction at a prestigious out-of-state institution, which resulted in a left and right hepatico-jejunostomy. After that, he suffered from multiple episodes of cholangitis and underwent right PTC stent placement and dilatations without any improvement.
Several surgical consultations at various other institutions concluded that surgery was not possible. Instead, stent replacement and antibiotics were recommended. Because of associated pain, the patient was also opioid dependent.
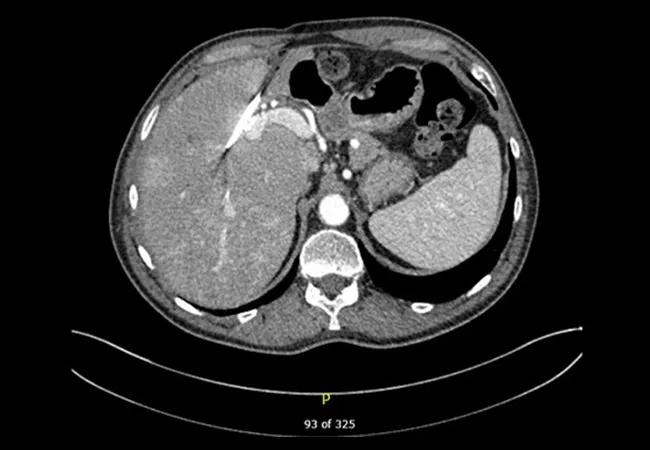
In April 2016, he presented to Cleveland Clinic where he was studied with both with an MRI and a CT scan (see main image above) that showed an atrophic left hepatic lobe, a right-sided internal-external percutaneous transhepatic biliary drainage catheter with mild segmental intrahepatic biliary dilatation in the right lobe, as well as a markedly atrophic left lobe. The left hepatic duct was completely obstructed and undrained.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5e454427-75fa-4225-9bec-59a102bdafb2/17-DDI-3797-Miller-CQD-Inset-1_jpg)
Preoperative MRI showing right hepatic duct dilation.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9d5e0eb2-50f2-4aa3-9851-c151e1bf8d0c/17-DDI-3797-Miller-CQD-Inset-2_jpg)
Postoperative cholangiogram showing patent hepaticojejunostomy without filling defects.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/af2333ad-cf6f-4b3f-851d-b57ec9ef732c/17-DDI-3797-Miller-CQD-Inset-3_jpg)
CT scan showing the liver after left hepatectomy with a new hepaticojejunostomy.
In May 2016, the patient underwent a left hepatectomy and removal of the entire left hepatic duct. The biliary drain on the right hepatic duct was exchanged on a wire and a short portion of the right hepatic duct was resected to fresh tissue. The right hepatico-jejeunostomy was also refashioned over a new stent.
Advertisement
The patient recovered uneventfully. One month after surgery, a cholangiogram showed a widely patent hepatico-jejunostomy and the biliary drain was removed.
At one-year follow-up, the patient was doing well with no more episodes of cholangitis and normal liver function. He no longer uses opioids.
References
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications