“It’s better for everyone,” surgeon says.
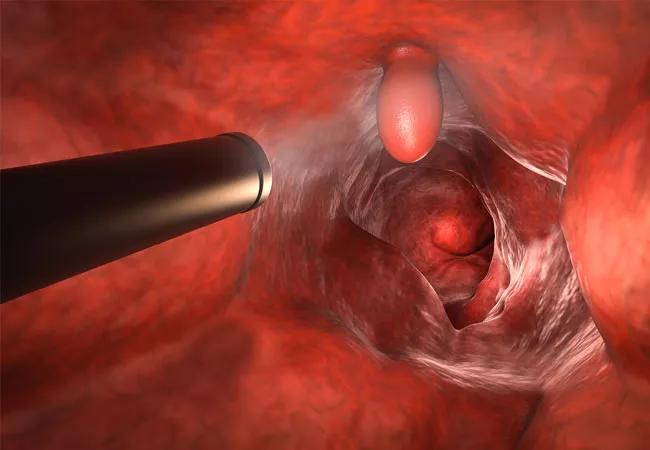
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/959618fd-6150-43e0-8dcd-c1ef7594342d/19-DDI-240_CQD_650x450_A_jpg)
Endoluminal Surgery
Cleveland Clinic is pioneering the use of advanced endoscopic techniques to remove complex polyps and early malignant lesions in the digestive tract without anesthesia. Selected colorectal procedures are now performed under conscious sedation in the outpatient Endoluminal Surgery Center.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We prefer to use conscious sedation when removing benign polyps and early malignant lesions that are low-risk for metastasis. Patients prefer it, outcomes are improved and procedures are less expensive,” says Cleveland Clinic colorectal surgical oncologist and endoluminal surgery pioneer Emre Gorgun, MD. “It’s really better for everyone.”
Conscious sedation is less risky than sedation with propofol or general anesthesia, particularly for patients with heart disease or other comorbid condition presenting for gastrointestinal surgery.
“Patients are able to roll over or move as requested and can adjust their own body position to remain comfortable. They awaken easily and quickly regain their balance and stability, making same-day homegoing safer,” he says.
Expansion of screening protocols has increased the number of patients diagnosed with nonmalignant lesions or early cancers of the colon and rectum. Traditionally, such patients are referred for surgery. The availability of endoluminal surgery and natural orifice approach is allowing a growing percentage of patients with complex colon polyps, large duodenal polyps, early esophageal cancers, gastric cancers and neuroendocrine tumors to undergo less-invasive treatment.
“In our practice, the risk of recurrence is low at 2 to 3%,” says Dr. Gorgun. “Because these patients may be at high risk for recurrence, we do a repeat scope and surveillance at six months, then follow up every three years.”
Early cancers can be managed endoluminally, so long as lymph node involvement is negligible or nonexistent.
Advertisement
“We resect these lesions en bloc and measure the depth of invasion. If it is less than 1000 micrometers, all is well. With deeper lesions the risk of lymph node involvement rises, and organ resection becomes more appropriate,” he explains.
Lesions that may leave a large defect when removed are selectively scheduled for endoscopic surgery with laparoscopic backup.
Dr. Gorgun foresees the rapid expansion of endoluminal surgery as operators gain experience and devices evolve to handle increasingly complex lesions.
Several models for learning the technique have been developed, and Dr. Gorgun offers courses at Cleveland Clinic and at national meetings. “It is demanding on operators’ skills, so the learning curve is fairly steep,” he says.
Cleveland Clinic is partnering with device manufacturers to improve the tools needed to refine endoluminal surgery, including better scopes, tools that will facilitate endoscopic suturing and more dexterous robots. “They will make suturing safer and enable us to tackle much larger lesions,” he says.
Dr. Gorgun feels that interest in endoluminal surgery will accelerate once the sentinel lymph node for metastatic cancers is discovered. “Sentinel lymph node biopsy is key,” he says. “Currently in this country, for every four colons removed for cancer, one is removed for a nonmalignant lesion. When we discover the sentinel node, endoluminal surgery will become even more useful.”
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality