Research from three pulmonologists is shining light on mechanotransduction and ECM signal processing in ways that could lead to new therapeutic options
Written by Brian Southern, MD, Mitchell Olman, MD and Rachel Scheraga, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
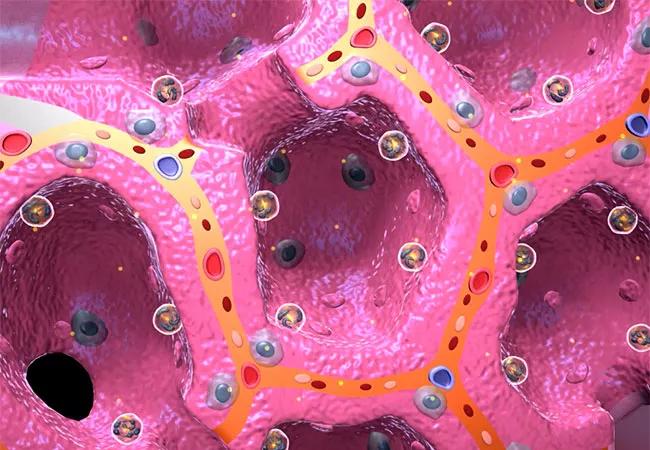
Pulmonary fibrosis results from progressive lung scarring that leads to air gas exchange and mechanical lung dysfunction. It is the end result of several unique disorders, with idiopathic pulmonary fibrosis (IPF) being the most common and the most severe with a three to five year median survival. IPF is considered secondary to an abnormal wound healing response to numerous subclinical micro-injuries. This results in deposition of excessive extracellular matrix (ECM) and leads to scar formation. At some point, the scarred lung ECM begins to trigger accumulation of fibroblasts and activation of fibroblasts into myofibroblasts. These scar-producing cells create a feed-forward mechanism which perpetuates fibrosis and disease progression. These ECM signals also affect the function of immune cells and have been shown to also play a role in the progression of inflammatory lung diseases such as acute lung injury and acute respiratory distress syndrome (ARDS).
We have known for many years that soluble cytokines and growth factors (e.g., transforming growth factor beta [TGF-β], Interleukin-1 beta [IL-β] and tumor necrosis factor alpha [TNF-α]) secreted by both parenchymal and immune cells can drive progression of fibrosis and/or inflammation. Emerging evidence now supports the idea that ECM microenvironmental signals, including the particular composition of ECM components, the architecture of the ECM (linear vs randomly arranged) or the stiffness of the ECM, can drive in accumulation and activation of fibroblasts. While current anti-fibrotic therapies target the effects of cytokines and growth factors, they only slow fibrosis progression (they do not stop or reverse it), and they do not take into account the interactions of fibroblasts with the underlying matrix. There are currently no specific therapies that are effective for ARDS. But increased understanding of how ECM microenvironmental cues influence cell behavior and perpetuate fibrosis and inflammation is leading to a paradigm shift in the pathogenesis of pulmonary disease that will likely lead to novel therapeutic strategies that can target these cell-matrix interactions.
Advertisement
The primary focus of our laboratories is understanding how immune cells and fibroblasts interact with the ECM. We study how the ECM stiffness signal is translated into a biochemical signal, a process known as mechanotransduction, and its consequences on cellular processes involved in fibrosis and inflammation. We look at how mechanotransduction can promote pulmonary disease progression in an attempt to develop new therapeutic targets to halt or reverse the disease process. Many published studies have utilized cells plated on glass or plastic, which is 1 million times stiffer than the lung. In contrast, our studies have found that utilizing conditions that resemble normal and fibrotic lung ECM stiffness yield results that differ substantially from prior work.
In 2014, the Olman lab published, for the first time, that the mechanosensing signal in fibroblasts is mediated by the transient receptor potential vanilloid 4 (TRPV4) channel, a surface membrane cation (calcium) channel that responds to changes in matrix stiffness. Using complementary in vitro and in vivo methods, we showed that targeting the TRPV4 channel can inhibit the ECM stiffness-mediated activation of fibroblasts and protect mice from experimental pulmonary. More recently in 2019, the Olman lab, spearheaded by Lisa Grove, PhD, published more detailed insights into the mechanism of TRPV4 signaling. We showed that TRPV4 is translocated to the cell surface where it acts as a
In 2016, Dr. Scheraga led work in the TRPV4 field by showing that mechanosensing through TRPV4 also regulated macrophage ingestion of bacteria in the context of increased ECM stiffness, such as that seen in lung in animal models of acute lung injury and infection. In contrast to the detrimental actions of TRPV4 in pulmonary fibrosis, Dr. Scheraga showed, using complementary methods, that TRPV4 is required for the induction of anti-inflammatory/pro-resolution cytokines, in vivo and in vitro macrophage ingestion of bacteria and consequent reduction in Pseudomona aeruginosa-associated lung injury in mice. In this context, TRPV4 in macrophages appears to be beneficial, and stimulating TRPV4 could reduce lung injury and increase bacterial clearance thereby resolving infection-associated ARDS.
Advertisement
Dr. Scheraga published some exciting work in 2019 which demonstrated that the mechanism of TRPV4’s regulation of macrophage activity in a mechanosensitive manner occurs through intracellular signals involving the mitogen activation protein kinase (MAPK) pathway. As mentioned above, targeting these specific molecular mechanisms downstream of TRPV4 could modulate the response in various disease states without affecting the overall function of TRPV4. These findings may have broad impact, as TRPV4 and macrophage activation functions are implicated in other inflammatory lung diseases including bronchiectasis, COPD, granulomatous lung diseases as well as vascular and malignant diseases.
Many clinical trials in pulmonary fibrosis tend to focus on individual soluble mediators or isolated pathways that play a role in fibrosis and have failed in the clinical setting. Identifying a potential therapeutic strategy that targets a molecule, such as non-muscle myosin II (NM-II), which is downstream and common to multiple fibrosis pathways could represent a significant paradigm shift in the treatment of patients with IPF and other fibrotic disorders.
Dr. Southern published novel work in 2016 on the role of fibroblast NM-II in responding to ECM cues such as stiffness and architecture. This work demonstrates that when fibroblasts encounter normal lung ECM, NM-II is activated in the periphery of the cell. This limits its lateral protrusive activity and helps the cell establish polarity, and it effectively promotes fibroblast migration. When the fibroblast encounters the stiff fibrotic lung, it becomes immobilized, and NM-II becomes activated diffusely throughout the cell, resulting in increased contractility and differentiation into a fully active myofibroblast.
Advertisement
Since then, Dr. Southern has focused on ways to manipulate the NM-II pathway in fibroblasts and has identified a protein that regulates NM-II movement within the cell. Blocking this protein restricts NM-II from localizing to central stress fibers in the fibroblast and prevents myofibroblasts differentiation, as well as pulmonary fibrosis in mice. This work is currently being submitted for publication, and it has the potential to shift the paradigm of treatment by focusing on manipulation of a common final pathway in fibrotic disorders that involves fibroblast matrix interactions.
Through the above work and that of a number of other labs, the understanding of the role of mechanotransduction and processing of other ECM signals has become an integral part of studying pulmonary diseases. Laboratory methods often must account for the stiffness of the substrates on which they perform their studies, as many of these proteins only respond to a finely-tuned range of stiffness, such as that seen in the normal and fibrotic lung. Culturing cells and organoids under pathophysiologic ECM conditions are just two examples of techniques that labs have incorporated around the world. Clinical trials that specifically target matrix stiffness (e.g., LOXL inhibitors) and mechanosensing pathways (e.g., ROCK inhibitors) are becoming more common. As we begin to elucidate how immune cells and fibroblasts respond to signals in their natural environment, the paradigm for understanding what drives progressive fibrosis or inflammation will continue to shift, and therapeutic options for patients with inflammatory or fibrotic lung disorders will continue to expand.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management