Insights on the practical application and limitations of a common test
By Parth Parikh, MD; Nishant Shah, MD; Haitham Ahmed, MD, MPH; Paul Schoenhagen, MD; and Maan Fares, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The United States has seen a decline in fatal myocardial infarctions, largely thanks to early detection of coronary artery disease. Current guidelines on assessment of cardiovascular risk still rely on the traditional 10-year risk model in clinical practice. However, the predictive value of this approach is only moderate, and many coronary events occur in people considered to be at low or intermediate risk.
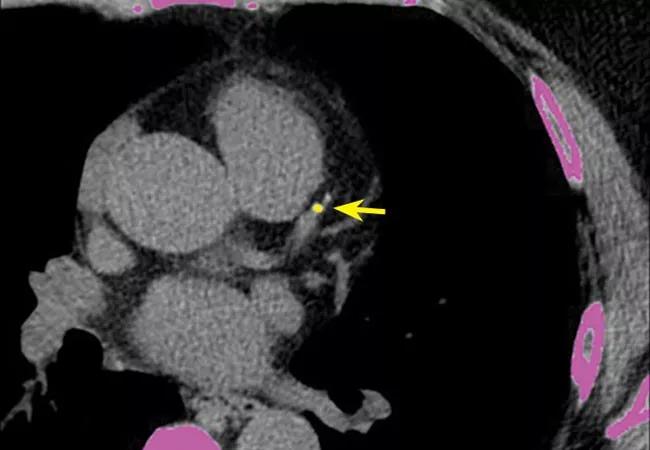
Coronary artery calcium scoring is useful in diagnosing subclinical coronary artery disease and has emerged as a means of risk stratification by direct measurement of disease. Many providers are using it, and its relatively low cost and ease of performance have contributed to its widespread use. However, downstream costs, radiation exposure and lack of randomized controlled trials have raised concerns.
This post, excerpted from a recent review article we published in Cleveland Clinic Journal of Medicine (2018;85:707-716), outlines our approach to determining who should be tested with coronary artery calcium scoring, with illustrative case vignettes, and what to do about an elevated score.
In the 2013 guideline on assessment of cardiovascular risk from the American College of Cardiology and American Heart Association (ACC/AHA),1 coronary calcium scoring has a class IIB recommendation in scenarios where it may appear that the risk-based treatment decision is uncertain after formal risk estimation has been done. According to a 2017 expert consensus statement2 and 2016 guidelines3 from the Society of Cardiovascular Computed Tomography, a coronary calcium score higher than 100 could be a rationale for starting aspirin therapy, and a score higher than 0 could be a rationale for statin therapy. Current guidelines also mention that the coronary calcium score is comparable to other predictors such as the C-reactive protein level and the ankle-brachial index.
Advertisement
Compared with the ACC/AHA guideline, the Society of Cardiovascular Computed Tomography guidelines and consensus statement added more specifics in terms of using coronary calcium testing for asymptomatic patients at intermediate risk (10-year risk of atherosclerotic cardiovascular disease, 5 to 20 percent) and in selected patients with a family history of premature coronary artery disease and a 10-year risk less than 5 percent.2,3 An earlier (2010) ACC/AHA guideline on cardiovascular risk assessment4 was more specific, offering a class IIA recommendation for patients at intermediate risk (Framingham Risk Score of 10 to 20 percent).
The 2013 ACC/AHA guideline cited cost and radiation exposure as reasons for not giving coronary calcium measurement a stronger recommendation.1 However, as data continue to accumulate, the guidelines may change, especially since low-dose radiation tools are being used for cancer screening (lungs and breast) and since the cost has declined over the past decade.
Given the negative predictive value of the coronary calcium score, our approach has been to use this test in asymptomatic patients who are found to be at intermediate risk of atherosclerotic cardiovascular disease based on the ACC/AHA risk calculation1 and are reluctant to start pharmacologic therapy, or who want a more personalized measure of coronary artery disease. This is preceded by a lengthy patient-physician discussion about the risks and benefits of the test.5
The patient’s risk can then be further clarified and possibly reclassified as either low or high if it doesn’t remain intermediate. A discussion can then take place on potentially starting pharmacologic therapy and/or intensive lifestyle modifications.5,6 If an electronic medical record is available, CT results can be shown to the patient in the office to point out coronary calcifications. Seeing the lesions may serve as an additional motivating factor as patients embark on primary preventive efforts.7
Advertisement
Below, we describe cases of what we would consider appropriate and inappropriate use of coronary artery calcium scoring.
A 55-year-old man presents for an annual physical and is found to have a 10-year risk of atherosclerotic cardiovascular disease of 7 percent, placing him in the intermediate-risk category. Despite an extensive conversation about lifestyle modifications and pharmacologic therapy, he is reluctant to initiate these measures. He is otherwise asymptomatic. Would calcium scoring be reasonable?
Yes, it would be reasonable to perform coronary artery calcium scoring in an otherwise asymptomatic man to help reclassify his risk for a coronary vascular event. The objective data provided by the test could motivate the patient to undertake primary prevention efforts or, if his score is 0, to show that he may not need drug therapy.
A 55-year-old man who has a family history of coronary artery disease, is an active smoker and has diabetes mellitus presents to the clinic with two months of exertional chest pain that resolves with rest. Would coronary artery calcium scoring be reasonable?
This patient is symptomatic and is at high risk of coronary artery disease. Statin therapy is already indicated in the ACC/AHA guidelines, since he has diabetes. Therefore, calcium scoring would not be helpful, as it would not change this patient’s management. Instead, he would be best served by stress testing or coronary angiography based on the stability of his symptoms and cardiac biomarkers.
Advertisement
A 30-year-old woman with no medical history presents with on-and-off chest pain at both exertion and rest. Her electrocardiogram is unremarkable, and cardiac enzyme tests are negative. Would coronary calcium scoring be reasonable?
This young patient’s story is not typical for coronary artery disease. Therefore, she has a low pretest probability of obstructive coronary artery disease. Moreover, calcium scoring may not be helpful because, at her young age, there has not been enough time for calcification to develop (median age is the fifth decade of life). Thus, she would be exposed to radiation unnecessarily at a young age.
Coronary artery calcification is now being incidentally detected as patients undergo CT for other reasons, such as screening for lung cancer based on the U.S. Preventive Services Task Force guidelines. Patients may also get the test done on their own and then present to a provider with an elevated score.
It is important to consider the entire clinical scenario in such patients and not just the score. If a patient presents with an elevated calcium score but has no symptoms and falls in the intermediate-risk group, there is evidence to suggest that he or she should be started on statin therapy, aspirin therapy or both.
An abnormal test result does not mean that the patient should undergo more-invasive testing such as cardiac catheterization or even stress testing, especially if he or she has no symptoms. However, if the patient is symptomatic, then further cardiac evaluation would be recommended.
Advertisement
Measuring coronary artery calcium has been found to be valuable in detecting coronary artery disease and in predicting cardiovascular events and death. The test is relatively easy to perform, with newer technology allowing for less radiation and cost. It serves as a more personalized measure of disease and can help facilitate patient-physician discussions about starting pharmacologic therapy, especially if a patient is reluctant.
Currently, coronary calcium scoring has a class IIB recommendation in scenarios in which the risk-based treatment decision is uncertain after formal risk estimation has been done according to the ACC/AHA guideline.1 The Society of Cardiovascular Computed Tomography consensus document is more specific in recommending the test in asymptomatic patients in the intermediate-risk group.2
Limitations of calcium scoring include the possibility of unnecessary cardiovascular testing, such as cardiac catheterization or stress testing, being driven by the calcium score alone, as well as the impact of incidental findings. With increased reporting of the coronary calcium score in patients undergoing CT for lung cancer screening, the score should be interpreted in view of the entire clinical scenario.
For the full review article from which this post was excerpted, see Cleveland Clinic Journal of Medicine (2018;85:707-716).
Drs. Parikh and Shah are fellows in the Departments of Internal Medicine and Cardiovascular Medicine at Cleveland Clinic. Drs. Ahmed, Schoenhagen and Fares are staff physicians in the Department of Cardiovascular Medicine.
Image at top reprinted from Cleveland Clinic Journal of Medicine (2018;85:707-716).
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more