Findings have implications for reducing venous thromboembolisms
Colorectal surgeons’ perception that postoperative enoxaparin therapy is too expensive for many patients after surgery for inflammatory bowel disease (IBD) could be limiting its use, although the treatment can reduce the formation of dangerous blood clots.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
New research from Cleveland Clinic colorectal surgeon and IBD Surgery Section Chief and Director of Research Stefan Holubar, MD, MS reveals, however, that the copay charges for enoxaparin prophylaxis are relatively small for most insured patients. The study findings were presented at the 2022 Digestive Disease Week annual meeting.
“One of the perceived barriers on some surgeons’ part was that these patients were routinely having excess out-of-pocket costs, that enoxaparin was not affordable and that patients were routinely getting stuck with a $200 bill,” Dr. Holubar says. “We found that not to be the case.”
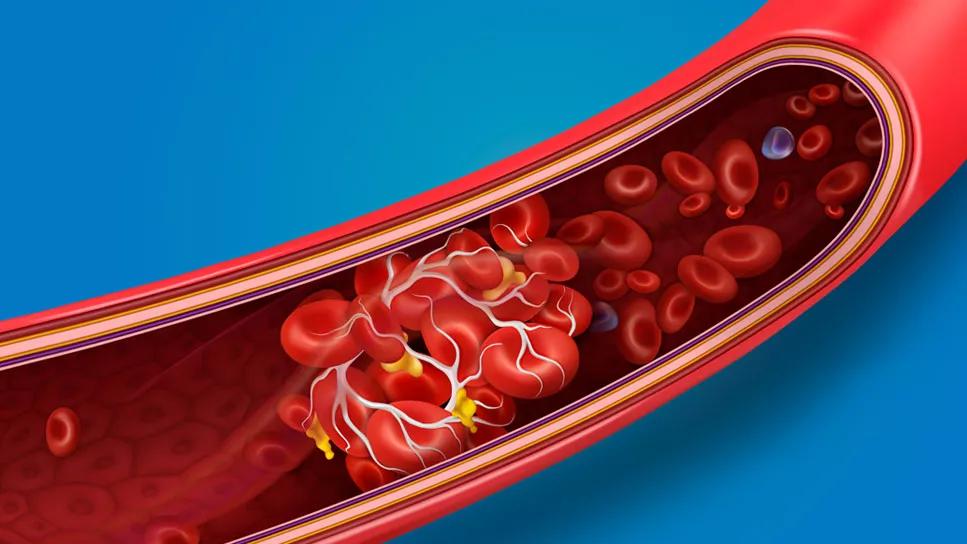
Patients with colorectal cancer and IBD, including those who undergo surgery, face an increased risk of venous thromboembolisms (VTEs), which can result in significant morbidity and mortality. Pathogenesis is unclear but is likely due to multiple factors including genetics, age, disease activity and hospitalization. About 40% of VTE events occur after a patient leaves the hospital, Dr. Holubar says.
Studies have shown that chemoprophylaxis can reduce the risk of symptomatic VTE by 70% to 80%.
As part of a National Surgery Quality Improvement Program project, Dr. Holubar and colleagues assessed the cost of extended-discharge chemoprophylaxis for a group of patients who underwent surgery for Crohn’s disease, ulcerative colitis or colorectal cancer at Cleveland Clinic in 2020 or 2021. At discharge 136 patients received enoxaparin and 31 received baby aspirin as extended chemoprophylaxis.
Advertisement
The overall mean copay cost of enoxaparin was $43.35. The mean copay for patients with private insurance was $29.27, $83.06 with Medicare coverage, $7.83 with Medicaid and $168.06 for patients who paid out of pocket.
Although a couple of patients paid $200 or more for enoxaparin — including one patient who paid $277 — those large copay amounts were outliers. Of the patients receiving aspirin, 16 did so because they could not afford their enoxaparin co-pay. The mean cost of a 36-day supply of enteric coated, 81 mg aspirin was $9.75.
“I was pleasantly surprised by the findings,” says Dr. Holubar. “They were reassuring. There was zero data on this topic, and our guesstimate was that 30% of the patients would have a substantial cost.” The study “puts to rest the myth that the perceived barrier of cost is an impediment for the majority of patients.”
Although the indication for extended-discharge enoxaparin in IBD surgery patients is relatively new, its use is increasing among colorectal surgeons at Cleveland Clinic, Dr. Holubar says. “Until something better comes along, we feel prescribing postoperative enoxaparin is a best practice.”
Patients are instructed on how to self-inject enoxaparin.
In the study cohort, three patients experienced a postoperative VTE and four required transfusions for significant bleeding within 30 days of surgery. None of the aspirin recipients experienced significant bleeding or a VTE after discharge.
The study included slightly more men, 51%. Mean age of participants was 46 years and mean body mass index was 26 kg/m2. The most common IBD diagnoses was Crohn’s disease in 38% of patients, followed by 27% with ulcerative colitis and 24% with either colon, rectal or anal cancer.
Advertisement
Ileocolic resection, total abdominal colectomy, and completion proctectomy with ileal pouch-anal anastomosis were the most common surgeries.
Dr. Holubar and colleagues are planning a future multicenter prospective study to evaluate if twice-daily, 81 mg aspirin is an appropriate option compared to enoxaparin. As a pill, aspirin is more convenient than an injection and costs less.
“Aspirin, a more cost-conscious option, may be a safe alternative chemoprophylactic agent which could help improve patient compliance,” the investigators noted.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years