Supporting newly graduated RNs before and after the pandemic

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e386106d-4818-4644-a621-bda5a7f1199a/CCC_5522210_01-03-25_017_SCG)
Nurse residency
By Joan Kavanagh, PhD, RN, NEA-BC, FAAN; Christine Szweda, MS, BSN, RN; and Kathryn Stuck Boyd, MSN, RN, NPD-BC
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lightning-fast advances in knowledge and technology present enormous opportunities for improving healthcare while the newly graduated RN preparation-to-practice gap continues to widen. As the pandemic hit, pre-licensure programs suddenly faced a steep new hurdle: how to help nursing students gain crucial experience when hospitals tightened restrictions to protect patients, caregivers, faculty and students.
The collective response from nursing educators has offered reasons for optimism. Nursing programs responded with creativity as they pivoted from presenting in-person classes and clinicals to virtual classes and truncated clinical experiences. When events forced innovation, nursing programs were nimble, and they demonstrated to future nurses — and to program leaders themselves — that they can adapt under intense pressure.
Flexibility under pressure will continue to be valuable after the pandemic, as we respond to the imperative to improve nurse competencies in an environment that is changing at warp speed.
At Cleveland Clinic’s Stanley Shalom Zielony Institute for Nursing Excellence, systems we have put in place to help newly graduated RNs improve competency and confidence are showing results that make a difference in care delivery and in the professional experiences of new nurses.
The ability of nursing graduates to think critically is a key to safety, particularly in the area of identifying changes in patients’ conditions, according to team.
Recognizing this need, deans from the nation’s schools of nursing affiliated with the American Association of Colleges of Nursing approved “The Essentials: Core Competencies for Professional Nursing Education,” setting competency expectations for graduates of baccalaureate and graduate-level nursing programs.
To support new graduate RN (NGRN) success, in 2014, Cleveland Clinic launched a competency- and evidence-based one-year residency, accredited with distinction by the American Nurses Credentialing Center in 2020. The residency follows what is typically a three-month orientation. During that time, each NGRN is paired with an experienced RN success coach. The success coaches are nurse professional development specialists who serve as liaisons between new nurses, their preceptor and the nurse manager.
Advertisement
During orientation, caregivers self-assess using a holistic proprietary tool that explores topics such as coping mechanisms, organizational and professional commitment, professional behavior, self-efficacy, and help-seeking behavior. The outcomes help the success coach anticipate and support the unique needs of each nurse.
Historically, Cleveland Clinic used the Performance-Based Development System©, which evolved into an artificial intelligence platform supported by HealthStream, called Jane, to assess critical thinking and identify newly hired nurses’ strengths and opportunities for growth. In the asset-based environment of Cleveland Clinic nursing education, Jane is referred to as the Success Navigator.
Perhaps one of the most powerful tools we have developed to advance new-nurse readiness is the Problem-Recognition Workshop.
Participation in the three-day immersive experience involves assessments to better understand if new-graduate nurses consistently recognize a change in a patient’s condition or understand the level of urgency. Failure or inconsistency in recognizing a change in patients’ conditions may result in a failure to escalate concerns or ask for help. The program employs an innovative framework for developing self-confidence, critical thinking and patient problem-recognition skills.
Based on Tanner’s model of clinical judgment, the Problem Recognition Workshop assumes and respects the knowledge individuals bring to the program. The workshop uses facilitated small-group case study and problem identification discussions that:
Advertisement
Nurses who fixate on irrelevant data are generally unable to identify the chief patient problem, so the ability to sift through patient information is key. Throughout the program, information is provided incrementally as the patient would exhibit a change in status throughout a nurse’s shift. The participant builds their SBAR reports as new information is provided, and at the end of the case study they are asked to share the problem they think the patient is experiencing.
The program begins with the use of video vignettes that present a patient who, over time, decompensates or declines in some way. Participants review the patient’s history, identifying what the patient may potentially be at risk for. Then, in small groups, participants use a proprietary exercise called the Dot Method (see sidebar) to identify the problem.
Prioritization exercises simulate a full patient assignment and give participants an opportunity to differentiate urgency, identifying who should be seen first and who is non-urgent.
Deductive reasoning and critical thinking patterns that were learned in the classroom are then applied in a virtual clinical environment. Participants review the unique de-identified chart of a real patient who was on a medical/surgical inpatient unit, including the most recent head-to-toe nursing assessment. Then they present an SBAR report to the small group which is debriefed to ensure the nurse has identified relevant data and accurately anticipated risks.
A low-fidelity simulation experience further develops the nurse’s ability to differentiate relevant from irrelevant data. Participants receive an overview of how to use manikins and are coached to incorporate the entire patient environment in their assessment to anticipate and plan for safe care. They independently identify the patient problem occurring and prioritize the scenario as urgent or non-urgent.
Advertisement
In another activity, nurses collect patient information by scanning QR codes that link to assessment findings or other clinical data points. This innovative strategy allows nurses to assess the patient in whatever order they feel appropriate.
The Problem-Recognition Workshop’s immersive, generative environment places nurses with peers of similar abilities to build confidence and competence in a nonthreatening, supportive atmosphere. Participants describe feeling completely comfortable asking questions in their small peer groups. The workshop helps nurses connect the pieces of data and pull relevant information from the stores of knowledge they have acquired through school and practice.
The program also encourages increased rapidity of the critical thinking process by subtly reducing the time frame allotted for answering questions. Participants progress so that they can proceed from SBAR review to assessment to final conclusion in a clinically realistic time of 10 minutes.
Designed by nurses for nurses, the Problem-Recognition Workshop reinforces standards for performance. There are strong indicators that the methods can be easily implemented in hospital and academic settings to improve anticipatory thinking, early recognition of patient problems and prioritization of patient needs. These skills contribute to safe practice and reflective thinking throughout one’s career.
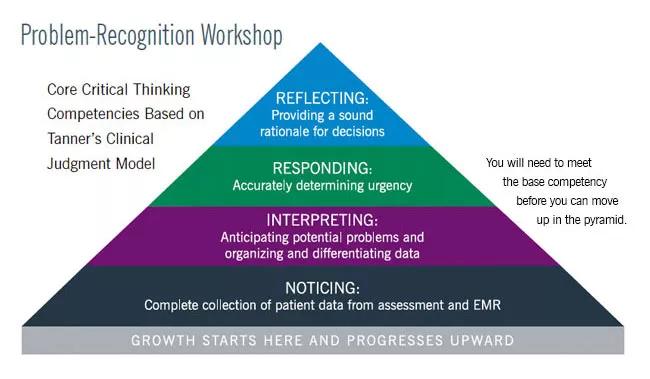
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4ca99ea3-cfbc-4937-90ac-b0473ace48fc/21-NUR-2197647-Creating-CultureOfSafetySuccess-CQD-inset_650x379-2_jpg)
The Dot Method visual management technique is somewhat similar to concept mapping. It helps nurses sort through data points to identify those that best correlate with the patient’s history and presentation and will lead to accurate problem recognition.
Advertisement
The dot metaphor applies as well to Cleveland Clinic’s Problem-Recognition Workshop as a whole, which can be likened to a pointillist painting. Standing up close to the painting on the wall of a museum, one sees discrete dots. Only by viewing the painting at a distance can one see the essence of the picture.
Advertisement
Strengthening outcomes through clear, transparent communication
Harnessing digital innovations to enhance nurse confidence and clinical outcomes
Regional organizations collaborate to address nurse faculty shortage
How wellness habits help nurses flourish
Planning continues with critical, patient-focused input from nursing teams
Strengthening care through targeted resources and frontline voices
Embracing generational differences to create strong nursing teams
CRNA careers offer challenge and reward