Pinpointing how tumors reprogram platelets and trigger blood clots
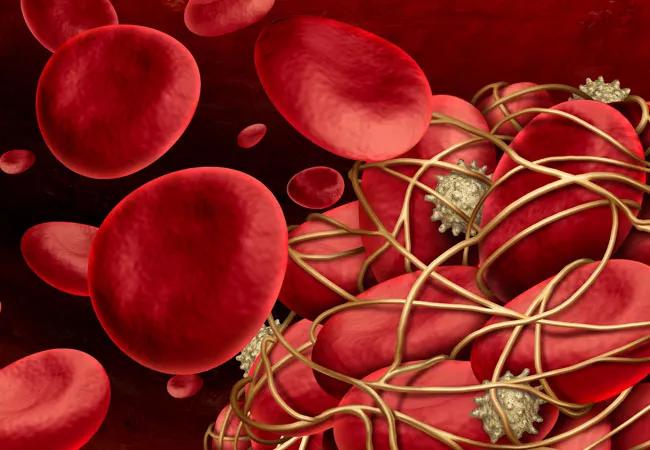
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/97f18215-25ba-4cb6-bded-6a7fd88f030f/23-CNR-4023808-CQD-Hero-650x450-blood-clots_jpg)
blood clots and cancer
Thrombosis is one of the leading causes of mortality for people with cancer, and often goes undetected. To date, little has been understood about the role of platelet activation in causing these complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Newly published research from Cleveland Clinic’s Lerner Research Institute explores the mechanisms of tumor-platelet communication and activation—yielding insights that could lead to therapies that protect patients with cancer from thrombosis.
The elevated risk of clotting complicates treatment, as patients with cancer are also more susceptible to bleeding and hemorrhage. Conventional treatments like blood thinners contribute to this risk. In addition to being a life-threatening risk in its own right, thrombosis increases the potential for cancers to metastasize, underscoring the critical need for the development of novel therapeutic approaches.
Small extracellular vesicles (sEVs) are associated with coagulation abnormalities in many conditions, including COVID-19 and many types of cancer, according to Tatiana Byzova, PhD, senior author of the paper. The study, led by Tejasvi Dudiki, PhD, explored the process by which sEVs in prostate, breast and renal cancer activate platelets. The researchers demonstrated platelet uptake of cancer cell-derived sEVs in vitro and in vivo via sEV-tetraspanin CD63, leading to platelet aggregation and blood clot formation.
Platelets accumulate cancer cell-derived mRNAs may serve as a predictive marker of coagulation abnormalities. In studying prostate cancer tumors, the researchers further discovered that an estimated 70% of patients exhibited a specific prostate cancer marker accumulating in their platelets. This accumulation disappeared after successful treatment involving the removal of the prostate gland.
Advertisement
An antibody developed in Dr. Byzova’s lab were designed to stop the interactions between platelets and tumor-derived sEVs. The goal of the patent-pending antibody is to prevent thrombosis that originates from cancer -sEVs uptake.
“Finding a balance between preventing blood clots and maintaining appropriate hemostasis is crucial to ensure patient safety,” says Dr. Byzova. “A more targeted approach is also essential for tailoring therapies to vulnerable patients, like older people who are more at risk for heart conditions.”
Learn more in our podcast episode about reduce thrombosis risk.
Advertisement
Advertisement
The relationship between MTHFR variants and thrombosis risk is a complex issue, but current evidence points to no association between the most common variants and an elevated risk
IV thrombolysis should not be delayed because of planned thrombectomy
Multi-site study reveals surprising findings
Aim is for use with clinician oversight to make screening safer and more efficient
Genetic variants exist irrespective of family history or other contributing factors
Percutaneous stabilization can increase mobility without disrupting cancer treatment
New guidelines update recommendations
Simple score uses clinical factors to identify patients who might benefit from earlier screening