Multiple endometriotic foci with complete bowel obstruction
A 49 year-old woman, with a history of pelvic endometriosis, presented with an eight-week history of progressively worsening abdominal pain, nausea and emesis. She was still passing flatus and described very small, effortful yet loose bowel movements daily. Previous endometriosis surgery included low anterior bowel resection and reanastamosis, excision of deeply infiltrating endometriosis and appendectomy 16 years ago.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Colonoscopy revealed normal looking colon. An ill-defined, mass-like lesion is visible on MRI, with tethering small bowel loops in the lower mid-abdomen and deep infiltrating endometriosis causing at least partial small bowel obstruction. MRI also revealed an additional foci of deep infiltrating endometriosis tethering the anterior rectal wall and a 2.4 cm left ovarian endometrioma. Bilateral hydrosalpinx was seen, and was greater on the right side.
In the following two weeks, the patient’s obstructive symptoms worsened and she began to feel nauseated. On physical exam, the patient’s abdomen is distended and tympanic, but soft. She was admitted, and CT of abdomen with oral contrast revealed progression of small bowel obstruction, secondary to endometriosis that occluded the distal small bowel. The patient received an NG tube, was rehydrated and prepared for emergency surgery.
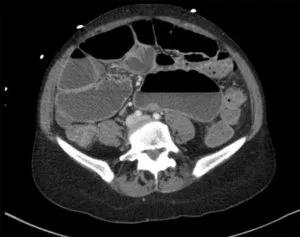
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/42c92b0d-bf44-40a8-b22b-466c16e96e7f/20-WHI-1844364_805x637_inset--300x237_jpg)
CT scan of the abdomen/pelvis revealed multiple, fluid-filled dilated loops on the bowel with transition point likely in the right lower quadrant secondary to infiltrating lesion.
Emergency laparotomy revealed a severely distended small bowel, and the entire distal ileum attached in loop-type formations toward a mass, which was located in the midline above the promontory. The small bowel had multiple obstructions in these areas, causing an ileus. The ileum was chronically dilated to a diameter of more than 7 cm for a length of more than 1 m, reaching up to the distal jejunum. Notably, only the proximal 90 cm of jejunum left unaffected by the severe ileus.
Advertisement
Recurrent endometriosis – potentially originating from the distal small bowel mesentery – had caused a complete obstruction, and the team felt that the bowel would perforate soon without surgical intervention. Additional endometriosis was seen between the uterus and neorectum.
“After consulting with a multidisciplinary team, including colorectal surgery, we opted to perform a comprehensive adhesiolysis and an extended ileocolic resection to completely remove the recurrent endometriosis of the bowel and to take the colon and neorectum off the uterus, followed by hysterectomy. We found the uterus was severely adhered to the colon,” says Cara King, DO, MS, Director of Benign Gynecologic Surgery for the Cleveland Clinic Ob/Gyn and Women’s Health Institute and Associate Program Director of the Minimally Invasive Gynecologic Surgery Fellowship.
“As a minimally invasive gynecologic surgeon, I generally manage endometriosis laparoscopically. However, in this particular case, the bowel obstruction and severe ileus necessitated open surgery. Given the extent of endometriosis in this patient, I have a difficult time calling it a benign disease. Endometriosis can worsen progressively, invading adjacent organs and tissues. Early diagnosis with the correct surgery is crucial in optimizing outcomes,” Dr. King continues.
The team carefully dissected the uterus off of the colon; however, unavoidable serosal tears occurred in the affected area of distal colon toward the colorectal anastomosis and upper rectum. These were ultimately oversewn and a side-to-side ileocolic anastomosis was created after bowel resection with diverting loop ileostomy.
Advertisement
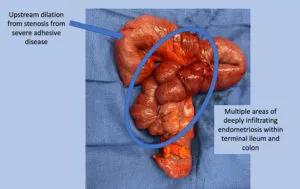
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fedadd70-e72d-4fcf-b347-af1291e9aef4/20-WHI-1844364_Endometriosis_inset-300x189_jpg)
The terminal ileum and colon with severe adhesions and stricture formation from deeply infiltrating endometriosis.
Pathology confirmed that all growths were benign, including:
Gastrointestinal involvement is found in one-third or fewer women with endometriosis, most commonly in the rectum and sigmoid colon. Involvement of the distal ileum is rare, and infrequently a cause of intestinal obstruction.
“Endometriosis is such a complex disease, in terms of both pathophysiology and surgical management. In cases of deep endometriosis, the involvement of a multidisciplinary surgical team is critical. We were able to combine our expertise in the surgical management of endometriosis and hysterectomy with the high-volume colorectal team — led by Hermann Kessler, MD, PhD — to lead the ileocolic resection. The team did a great job, with viable margins that were negative for endometriosis,” Dr. King concludes.
The patient was discharged home on postoperative day nine, without any adverse events. Her bowel symptoms have resolved. She is scheduled to have her ileostomy reversed approximately three months postoperatively.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications