Symptoms indicate tumor location
By Alberto J. Montero, MD, MBA
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Primary care physicians play a vital role in detecting cancers at earlier stages and synthesizing information from a patient’s presentation, vital signs, physical examination and results of laboratory and radiographic testing. This post provides clinically relevant colorectal cancer pearls from an oncologic perspective for primary care physicians.
With an estimated annual incidence of 132,700 cases diagnosed in the United States in 2015, colorectal cancer is the third most common cancer.
National guidelines that recommend colonoscopy (starting at age 50 for people at standard risk) have had a significant impact on early detection rates and have translated into a significant decrease in mortality rates.
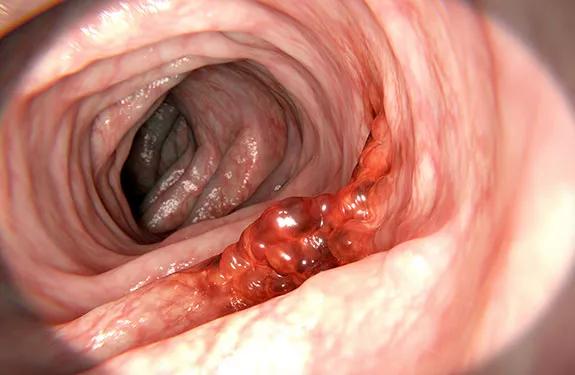
In symptomatic cases, clinical manifestations differ depending on tumor location.
Left-sided tumors can present with hematochezia, colicky abdominal pain and a change in bowel habits. And because the descending (left) colon has a smaller lumen than the right and tumors typically are annular in shape, left-sided cancers may present with abdominal distention with or without bowel obstruction or nausea and vomiting.
Right-sided tumors typically present with iron deficiency anemia from unrecognized blood loss.
Tumors near the rectum can cause tenesmus, rectal pain and diminished caliber of stools.
In the United States, 20 percent of colorectal cancer patients have distant metastases at the time of diagnosis, and the most common sites are the lymph nodes, liver, lungs and peritoneum.
Advertisement
Uncommon presentations of colorectal cancer include pneumaturia, fecaluria or recurrent urinary tract infection from a fistula, bacteremia with Streptococcus bovis or Clostridium septicum, and intra-abdominal abscess from a localized bowel perforation.
Once cancer is suspected, colonoscopy is the most accurate and versatile diagnostic test. It not only permits localization and biopsy of lesions throughout the large bowel, but also detects synchronous neoplasms and permits removal of polyps. Computed tomographic (CT) colonography is an alternative if colonoscopy is contraindicated, but it can only detect larger (> 6 mm) tumors.
According to the American Cancer Society (ACS), men and women at average risk should undergo colorectal cancer screening beginning at age 50. ACS screening recommendations for polyps and colorectal cancer include flexible sigmoidoscopy every five years, colonoscopy every 10 years, double-contrast barium enema every five years, or CT colonography every five years. Tests that detect cancer but not polyps include guaiac-based fecal occult blood test (every year), fecal immunochemical test (every year) and stool DNA test (every three years). These recommendations are fairly consistent with those of the National Comprehensive Cancer Network and U.S. Preventive Services Task Force.
Dr. Montero is staff in the Department of Solid Tumor Oncology.
This post is adapted from and contains part of an article that originally appeared in Cleveland Clinic Journal of Medicine. Read the full article for pearls on other types of cancer.
Advertisement
Advertisement

Emerging evidence suggests a patient-specific approach

Not if they meet at least one criterion for presumptive evidence of immunity

Essential prescribing tips for patients with sulfonamide allergies

Confounding symptoms and a complex medical history prove diagnostically challenging

An updated review of risk factors, management and treatment considerations

OMT may be right for some with Graves’ eye disease

Perserverance may depend on several specifics, including medication type, insurance coverage and medium-term weight loss

Abstinence from combustibles, dependence on vaping