Not if they meet at least one criterion for presumptive evidence of immunity
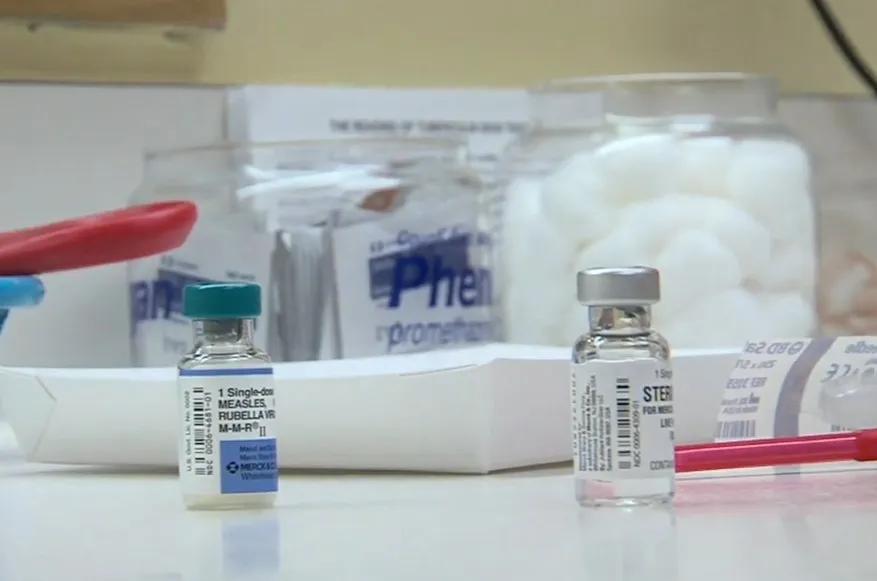
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b21bddb2-b3c1-4723-bfff-4fc701712a8b/MMR-vaccine)
MMR vaccine
By Kaitlyn R. Rivard, PharmD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This article is reprinted from the May 2025 issue of Cleveland Clinic Journal of Medicine (2025 May 1;92(5):279-282).
Does your adult patient need a measles vaccine? Possibly. Two doses of the measles-mumps-rubella (MMR) vaccine are recommended for children.1 Many adults (19 years and older) have preexisting immunity to measles from prior infection or vaccination. Adults without acceptable presumptive evidence of immunity to measles are recommended to receive one dose of MMR. Two doses of MMR are recommended for adults in special situations.1
Measles was eliminated from the U.S. in 2000.2 However, communities with reduced vaccination rates remain vulnerable to measles infection or outbreaks. As of April 18, a total of 800 confirmed measles cases have been reported in the U.S. this year,3 exceeding the 285 cases reported in all of 2024. The rising number of measles cases has garnered public attention and highlights the importance of vaccination in children and adults.
Before a vaccine became available, measles was considered a routine childhood illness and nearly everyone was infected by adulthood.2 About 500,000 measles infections were reported annually, although the U.S. Centers for Disease Control and Prevention (CDC) estimates that the actual number of cases was much higher, at 3 to 4 million per year.2,4 Annually, there were an estimated 48,000 hospitalizations, 1,000 cases of encephalitis, and 400 to 500 deaths attributed to measles. With the development and approval of a measles vaccine in 1963, a national vaccine campaign was launched, leading to the elimination of measles in the U.S. several decades later.2,4
Advertisement
A steep decline in measles cases was observed after a single-dose measles vaccine for infants was introduced. By the 1980s, annual reported cases of measles dropped below 4,000, but outbreaks continued to occur in vaccinated school-age children.2,3 To address the potential for primary vaccine failure (i.e., failure to produce protective antibodies after vaccination), the CDC recommended a second dose of measles vaccine before school entry starting in 1989.2 After high measles vaccination rates were achieved and maintained in preschool- and school-age children, measles was declared to be eliminated from the U.S. in 2000.2
Since measles elimination, isolated cases and small outbreaks have occurred, but these have been traced to sources originating outside the U.S. These outbreaks have historically been contained because vaccination rates among school-age children met or exceeded the threshold for herd immunity (95%), halting the chain of transmission.5 Because measles is one of the most contagious diseases in the world — one person with measles will infect 90% of susceptible contacts — outbreaks are hard to contain in predominantly unvaccinated communities.4
Disruptions in routine healthcare during the COVID-19 pandemic paired with an increasing prevalence of vaccine hesitancy have negatively impacted measles vaccination rates. In 2024, the national two-dose MMR vaccination rate in school-age children was 92.7%, and state vaccination rates varied widely, ranging from 79.6% in Idaho to 98.3% in West Virginia.6 The U.S. is increasingly vulnerable to larger-scale measles outbreaks as vaccination rates decline.
Advertisement
The live attenuated measles vaccine is highly effective in preventing measles infection by inducing both cell-mediated and humoral immunity.7,8 Because cell-mediated immunity is challenging to measure and interpret, humoral immunity (measles-specific immunoglobulin [Ig] G) is used to assess response in the clinical setting. With one dose of live attenuated measles vaccine, 96% of recipients will seroconvert to measles IgG positive, and nearly 100% will seroconvert with two doses.7
The live attenuated measles vaccine is considered to provide lifelong immunity when administered to children at age 12 months or older.7 Long-term studies demonstrate persistence of measles IgG for at least 11 years following one dose and at least 15 years following two doses.7,8 In people with waning or low-level measles IgG in the years following vaccination, protection is maintained due to cell-mediated immunity and an anamnestic immune response following subsequent measles exposure.7-9 While secondary vaccine failure (i.e., measles infection in a vaccine responder) is possible, it is exceedingly rare (< 0.2%) regardless of whether one or two doses are administered.9 Given the overall low incidence of measles infection in the U.S., serologic screening to identify the 4% of adults who do not seroconvert after one dose of a live attenuated measles vaccine is unlikely to provide an incremental benefit.
The combination live attenuated MMR vaccine is used in place of single-antigen component vaccines in the U.S. MMR vaccine may be given on the same day with other injectable or intranasal live virus vaccines (e.g., varicella). If administered on separate days, a minimum 28-day interval is required to prevent interference with the immune response.10 When MMR vaccination is administered as a two-dose series, the minimum interval between doses is also 28 days.
Advertisement
The MMR vaccine is recommended as a routine childhood vaccination.1,7 All children should receive two doses prior to school entry — the first dose at 12 months and the second dose between 4 and 6 years. The second dose may be given at an earlier age, spaced at least 28 days from the first dose.
Many adults have preexisting immunity to measles from previous infection or vaccination. Adults who meet at least one of the following four criteria are considered to have acceptable presumptive evidence of measles immunity7:
Advertisement
Adults born in or after 1957 who do not meet at least one of these criteria for acceptable presumptive evidence of immunity to measles should receive one dose of MMR vaccine.1,7 Adults recommended to receive two doses are described below. Adults born before 1957 are presumed to be immune to measles, but one dose of MMR vaccine can be administered if the patient requests it.
International travel. Infants 6 to 11 months should receive one dose of MMR vaccine before international travel and then also receive two doses after age 12 months (one dose after 12 months and a second dose at 4 to 6 years).1,7
For children older than 12 months and for adults who do not have acceptable presumptive evidence of immunity to measles, completion of the two-dose MMR series is recommended before international travel.1,7
Adult two-dose MMR vaccination. Adults who do not have acceptable presumptive evidence of immunity to measles should receive two doses of MMR vaccine in the following scenarios1,7:
Outbreaks. During a measles outbreak, state and local health departments will identify those at risk for exposure based on the epidemiology of the outbreak (i.e., if a specific age group or community is affected) and confirm adequate vaccination or other acceptable presumptive evidence of immunity to measles. Healthcare providers should continue to follow the routine recommendations for MMR vaccination unless additional guidance is provided by public health officials. In general, “booster” doses of the MMR vaccine are not recommended for adults meeting at least one criterion for acceptable presumptive evidence of immunity to measles. Infants 6 to 11 months should be vaccinated only in response to a measles outbreak if recommended by public health officials.7
Serologic screening is not recommended for people with at least one criterion for acceptable presumptive evidence of immunity to measles. In fact, documentation of adequate measles vaccination supersedes the results of postvaccination serologic testing,7 because serologic testing after vaccination is more likely to reflect waning humoral immunity than primary vaccine failure in an adult with a remote history of vaccination.
Prevaccination serologic screening can be considered, but is not required, in adults who do not have presumptive evidence of immunity to measles. For example, a clinician may test for measles IgG in adults vaccinated between 1963 and 1968 who may have received the inactivated measles vaccine, and then administer the MMR vaccine to those who test negative. Or clinicians may choose to administer MMR vaccine to all patients in this scenario, without measles IgG testing.
Detailed information on indications for the MMR vaccine specific to people who are not immune to rubella or mumps can be found on the CDC’s Adult Immunization schedule.1
Allergy. The MMR vaccine is contraindicated in people with a history of severe or anaphylactic allergy to the vaccine or a component, including neomycin. Patients with a history of nonsevere allergy to neomycin (e.g., contact dermatitis) can receive the vaccine, and it is safe to administer the vaccine to patients with egg allergy, regardless of allergy severity.7
Pregnancy. MMR vaccine is contraindicated in people who are pregnant or trying to become pregnant due to the theoretical risk of vaccine-induced congenital rubella syndrome. Women should be counseled to avoid becoming pregnant for 28 days after vaccination.7
Immunosuppression. MMR vaccine is contraindicated for individuals with immunocompromising conditions or those who are receiving immunosuppressive medications as there have been case reports of vaccine-induced infection.7 For a detailed list of immunocompromising conditions and therapies, refer to the altered immunocompetence section of the CDC’s General Best Practices for Immunization.10
MMR vaccine can be administered safely to children or close personal contacts of people who are pregnant or immunocompromised.7
MMR vaccine is typically well tolerated; the most common reactions reported in adults are fever (< 15%), transient rash (5%) and lymphadenopathy (20%).7 In children, the vaccine is associated with a small risk of febrile seizures (one case per 3,000 to 4,000 doses). In postpubertal females who are not immune to rubella, MMR vaccine is associated with a 25% incidence of mild arthritis-like symptoms, which present one to three weeks after vaccination and persist for an average of two days.7
For a list of references, see the original article in Cleveland Clinic Journal of Medicine (2025 May 1;92(5):279-282).
Dr. Rivard is a pharmacy clinical specialist at Cleveland Clinic.
Advertisement
Findings challenge the current diagnostic criteria for congenital Zika syndrome, expanding the definition beyond skull or brain abnormalities
Chemicals in e-cigarettes weaken the epithelial barrier in airways
Persistent rectal pain leads to diffuse pustules
Use of MRI adds to cost but remains cost-effective due to higher sensitivity
Anti-viral immunity identified a novel mechanism in necroptosis
Additional fine-tuning and recruiting of new patient groups underway
Using sequencing data to identify novel factors linked to kidney disease with unknown origin
Revised process helps prevent errors, streamline documentation