MRI classifier identifies a subset of patients with disease marked by cortical atrophy, not demyelination
New research from Cleveland Clinic is challenging long-held assumptions about the pathogenic mechanisms behind disability in progressive multiple sclerosis (MS). The findings suggest that permanent neurological disability can develop independent of cerebral white matter demyelination in a considerable subset of patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The research, led by the lab of Bruce Trapp, PhD, and published in Acta Neuropathologica (2024;148:34), involved development and validation of an MRI classifier that successfully identified myelocortical MS (MCMS), a variant characterized by minimal cerebral white matter demyelination despite significant disability. When applied to living patients with progressive MS, the classifier revealed that 22% demonstrated disability progression with minimal cerebral white matter demyelination. The findings are the first to correlate pathologically confirmed cortical atrophy and neurological disability.
The investigation stemmed from previous observations that immune-modulating therapies, while effective at reducing gadolinium-enhanced lesions and clinical relapses, show limited impact on disability progression. Additionally, earlier research by Dr. Trapp’s group and others had identified that T2 lesion volume explains less than 30% of brain atrophy variance and found that 45% of T2-weighted lesions in secondary progressive MS postmortem brains remain myelinated. Compared with aged-matched control brains, cortical neuronal loss was similar in cases with and without cerebral white matter demyelination.
The study employed a multiphase approach:
Advertisement
Development of the MRI classifier was a collaboration between the labs of Dr. Trapp and brain imaging research scientist Kunio Nakamura, PhD, both in Cleveland Clinic Lerner Research Institute.
The researchers made several significant discoveries:

Image content: This image is available to view online.
View image online ( https://assets.clevelandclinic.org/transform/ce35fc77-e54f-41dc-8799-fd125bff547a/ms-disability-independent-of-demyelination-inset)
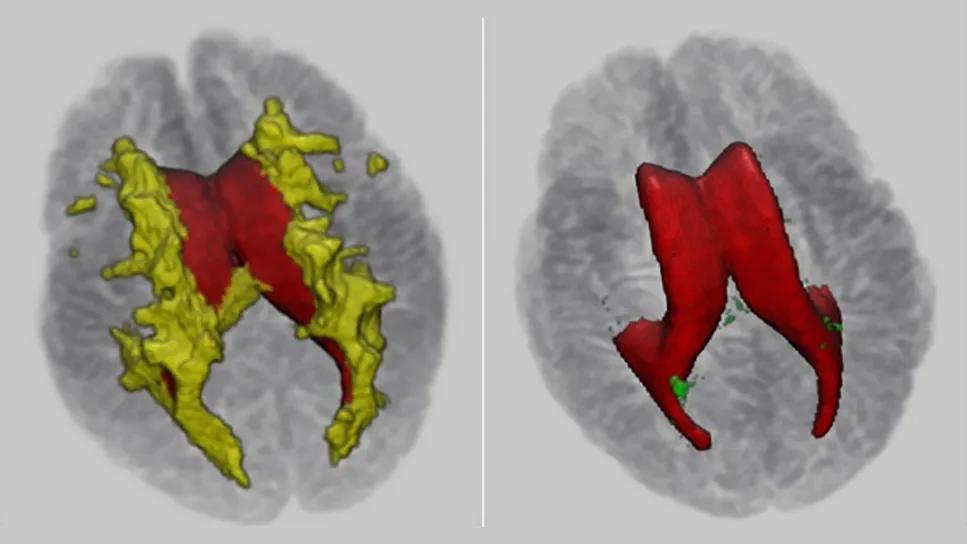
Three-dimensional maps of T2 hyperintensities (yellow) and T1 hypointensities (green) in postmortem typical MS (TMS) and myelocortical MS (MCMS) brains. T1 hypointensities were abundant in TMS and rare in MCMS. Reprinted from Singh V, et al. Acta Neuropathol. 2024;148:34, under a Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
The researchers note that their findings have substantial implications for both clinical practice and research:
Advertisement
“Now that we have further solidified that cortical atrophy is the best correlate of neurological disability in progressive MS patients, it is critical to prioritize researching cortical atrophy’s relationship with MS to the same degree that we focused on demyelination over the past 30 years,” says Dr. Trapp, the study’s senior author and Chair of the Department of Neurosciences. “We need to pivot as a research community. A lot of resources will be required, and many different approaches, to figure out why exactly the MS brain shrinks as it does.”
“Our research shows that a significant number of people with MS may have less white matter demyelination than previously thought,” adds co-author Daniel Ontaneda, MD, PhD, Director of Research for Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “Instead, these patients’ symptoms may be caused by different mechanisms, including injury to the cortical gray matter and spinal cord. Our findings have critical implications for clinical trials, especially those focused on remyelination of white matter lesions, and more generally for how people with MS accumulate disability.”
Dr. Ontaneda says more accurate inclusion of disease types in clinical trials will improve the outcome measures for potential treatments. Dr. Trapp is hopeful a potential treatment could target whatever is causing the cortical atrophy in the first place, and then be used in combination with existing medications primarily prescribed for relapsing MS.
Advertisement
“We’re talking about transforming a fundamental aspect of MS pathogenesis that has dominated MS research for decades,” Dr. Trapp concludes. “But now that we and others have pinpointed the vital focus area of cortical atrophy, that’s a significant hurdle cleared. I’m hopeful we all can collectively shift our research focus and delve into studying cortical atrophy’s relationship to MS.”
Advertisement
Advertisement

Mixed results from phase 2 CALLIPER trial of novel dual-action compound

A co-author of the new recommendations shares the updates you need to know

Rebound risk is shaped by patient characteristics and mechanism of action of current DMT

First-of-kind prediction model demonstrates high consistency across internal and external validation

Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

This MRI marker of inflammation can help differentiate MS from mimics early in the disease

Focuses include real-world research, expanding access and more