Novel insights from a postmortem study combining imaging, pathology and clinical perspectives
For physicians treating multiple sclerosis (MS), understanding the mechanisms behind progressive disability can be an elusive goal. While disease-modifying therapies have significantly impacted inflammatory disease activity and relapses, disability often accumulates independently, particularly in progressive forms of MS. The spinal cord plays a key role in this process, with its involvement predicting a progressive disease course and contributing to significant functional impairment. However, conventional clinical MRI of the spinal cord is limited in its ability to detect subtle yet crucial pathological changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
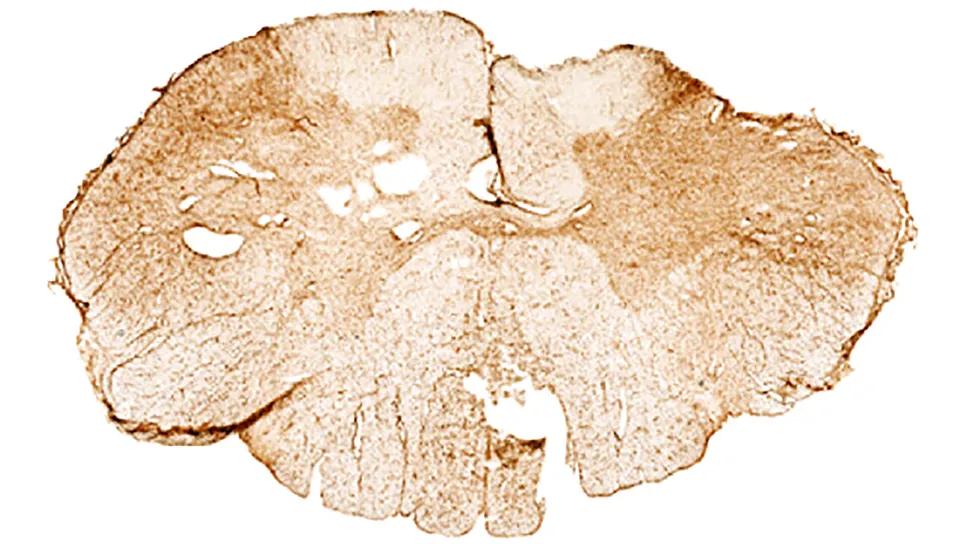
Now, a Cleveland Clinic study published in Neurology (2025;104:e210259) has shed new light on the intricate pathology within the MS spinal cord. By combining 7T postmortem MRI with detailed immunohistochemical analysis, investigators identified neurodegenerative changes occurring even in regions that appear myelinated on conventional MRI, offering insights into the heterogeneity of spinal cord pathology in MS and its correlation with clinical disability.
“We demonstrated that T2*-weighted MRI was able to discriminate demyelinated spinal cord lesions from T2*-hyperintense/myelinated and normal-appearing regions,” says the study’s lead author, Kedar Mahajan, MD, PhD, a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “We also found that T2*-hyperintense/myelinated lesions may be a window into neurodegenerative changes that may precede irreversible axonal loss in some individuals with MS and a progressive disease course.”
The study stemmed from the recognition that while spinal cord atrophy and T2 hyperintensities are contributors to disability in MS, they do not fully capture the underlying pathological complexity. Current clinical spinal cord imaging, often performed at 1.5T or 3T, is hampered by factors such as distance from the coil, motion artifacts and limited resolution, potentially masking subtle but significant tissue damage. Moreover, cord atrophy, a marker of irreversible axonal loss, often appears late in the disease process.
Advertisement
Dr. Mahajan and colleagues across Cleveland Clinic — in the Mellen Center (Daniel Ontaneda, MD, PhD), Department of Neurosciences (laboratory of Bruce Trapp, PhD), Department of Biomedical Engineering (laboratory of Kunio Nakamura, PhD) and the Lerner Research Institute Small Bore 7T MRI Core Facility (Caroline Androjna, DEng) — hypothesized that using ultra-high-field 7T MRI on postmortem spinal cord tissue, coupled with detailed pathological examination, would enable detection of a more heterogeneous spectrum of cord pathology than is apparent with clinical in vivo imaging alone. Their study aimed to evaluate the effectiveness of 7T MRI in discriminating different types of spinal cord pathology, to understand the relationship between these distinct MRI abnormalities and clinical disease characteristics, and to compare findings with clinical and lower-field postmortem MRI scans.
The study employed a cross-sectional design, analyzing postmortem cervical cord segments obtained from 40 individuals with MS enrolled in Cleveland Clinic’s MS Rapid Autopsy Program and 9 controls without MS.
A comprehensive multimodal approach was used. First, in situ postmortem MRIs (1.5T or 3T) of the brain and cervical spine were performed. Then 2-cm cervical cord segments were carefully selected, and high-resolution 7T MRI was conducted ex vivo. Some of the subjects had in vivo cervical spine MRIs available for comparison.
The cord segments then underwent detailed immunohistochemical analysis to quantify myelin, axonal density and size, and presence of activated microglia/macrophages. Quantitative T2* relaxation times were then correlated with these pathological markers and with clinical data, including Expanded Disability Status Scale (EDSS) score and upper cervical cord area (measured on in situ MRI brain scans).
Advertisement
7T MRI effectively discriminated demyelinated lesions, with a specific T2* threshold showing high accuracy, sensitivity and specificity. Notably, not all T2* hyperintensities corresponded to demyelination. Some regions, despite appearing abnormal on 7T T2* imaging, retained myelin. These were classified as T2*-hyperintense/myelinated regions.
Further immunohistochemical analysis revealed that these T2*-hyperintense/myelinated regions showed significant neurodegenerative changes compared with normal-appearing white matter. Specifically, they exhibited reduced axonal counts and increased axonal size, as well as increased levels of activated microglia/macrophages.
“While spinal cord atrophy has long been considered a predictor of progression in MS, this is inherently retrospective — by the time atrophy is detectable, axonal loss has already occurred,” Dr. Mahajan explains. “The true challenge lies in identifying biomarkers of neurodegeneration before irreversible structural loss occurs. This work challenges the prevailing notion that spinal cord hyperintensities merely reflect demyelination, and suggests the potential to capture earlier neurodegenerative processes within the MS spinal cord before irreversible axonal loss occurs.”
Interestingly, the study found that T2*-hyperintense/demyelinated lesions correlated significantly with both higher EDSS scores (indicating greater disability) and reduced upper cervical cord area (a measure of atrophy). In contrast, the T2*-hyperintense/myelinated regions did not show these strong correlations. Additionally, while demyelinated spinal cord lesion volume showed a weak correlation with brain T2* lesion volume, the myelinated hyperintense regions did not correlate with brain MRI measures. “In terms of clinical impact, spinal cord atrophy — even when localized — is likely the most significant, followed by demyelinated lesions and then more subtle neurodegenerative changes,” notes Dr. Mahajan.
Advertisement
Comparison with clinical 1.5T MRI and postmortem 3T MRI revealed that 7T MRI was more sensitive in detecting white matter T2* hyperintensities corresponding to demyelination, although many lesions were more conspicuous on axial than sagittal planes. The subtle T2*-hyperintense/myelinated regions were often not visible on the lower-field in vivo or in situ scans.
The study also observed a variable pattern of microglia/macrophage activation within both demyelinated and myelinated regions with neurodegenerative changes, suggesting various roles for these immune cells in different pathological contexts.
The findings led the authors to several key conclusions:
“The identification of these myelinated regions with T2* hyperintensity is an important step forward,” notes Dr. Mahajan. “It provides a novel opportunity to detect axonal pathology before significant axonal loss, or atrophy, occurs. This may open a window for earlier therapeutic intervention targeting compartmentalized (innate microglial/macrophage) inflammation and neuroprotection.” The authors also note that their findings spotlight the need for improved spinal cord imaging protocols in clinical practice, potentially including better axial coverage to avoid missing subtle lesions.
Advertisement
Dr. Mahajan and his co-authors have now translated these findings to a National Institutes of Health/National Institute of Neurological Disorders and Stroke-funded study that seeks to identify neurodegenerative features in vivo in patients at the Mellen Center using 7T MRI of the cervical spine. The study is being conducted in partnership with Cleveland Clinic’s Imaging Institute (Mark Lowe, PhD; Ken Sakaie, PhD; and Sehong Oh, PhD). “This could allow for earlier identification, in living patients, of these neurodegenerative changes that can precede irreversible axonal loss/spinal cord atrophy,” Dr. Mahajan says. “It could also help us monitor the effectiveness of neuroprotective strategies and increase the specificity for identifying demyelination to evaluate remyelinating therapies.”
Image at top reprinted from Mahajan et al. (Neurology. 2025;104:e210259) under terms of the Creative Commons CCBY-NC-ND license. © 2025 The Authors.
Advertisement

Mixed results from phase 2 CALLIPER trial of novel dual-action compound

A co-author of the new recommendations shares the updates you need to know

Rebound risk is shaped by patient characteristics and mechanism of action of current DMT

First-of-kind prediction model demonstrates high consistency across internal and external validation

Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

This MRI marker of inflammation can help differentiate MS from mimics early in the disease

Focuses include real-world research, expanding access and more