How we eliminated this common but unnecessary practice
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
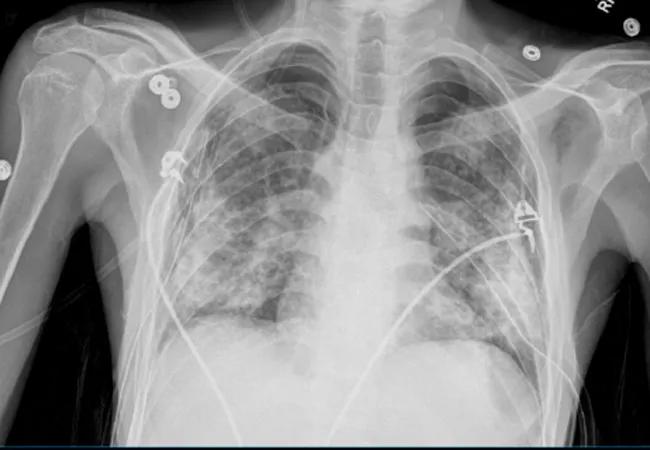
Many hospitals obtain chest X-rays (CXR) daily on patients in their intensive care units (ICU), though it has been over a decade since this practice was recommended. The American College of Radiology (ACR) stopped recommending daily CXR in 2008 after much research showed that using on-demand imaging does not impact ICU length of stay, duration of mechanical ventilation, morbidity or mortality, and can negatively affect patients’ sleep and radiation exposure rates. The ACR strengthened its stance on daily CXR to “usually not appropriate” in 2011 and 2014.
But for most clinicians and hospitals, including Cleveland Clinic, daily CXR remained standard practice. We averaged 375 portable CXR per day across the health system in 2018. Given the data supporting on-demand images, we sought to move away from this practice across all Cleveland Clinic hospitals.
Our first step was to meet with all key stakeholders, including intensivists, surgeons, pulmonologists and radiologists. We then altered the options for chest imaging in the electronic health record so that providers could only order daily CXR for patients with cardiac support devices or who had undergone cardiac and thoracic surgery. Providers were also required to indicate a specific reason for the need in this population. We analyzed data from the pre- and post-intervention periods with a two-sample t-test.
Average daily portable CXRs decreased 23.5 percent overall (P < 0.001), and average overnight CXR decreased 36.6 percent (P < 0.001). The CXR volume during rounding hours did not increase in compensation, and actually decreased by 15.8 percent (P < 0.001). The initiative did not result in any reported harm events or delays in care. I presented these results at the 2019 Society of Critical Care Medicine Annual Congress.
Advertisement
In the next phase of our project, we will continue to provide feedback to ICU directors about which providers are utilizing portable daily CXR. We also plan to reassess the need for daily CXR in cardiothoracic surgery and ICU patients to determine whether certain populations of patients may not benefit from this monitoring, and whether timing can be less disruptive to sleep for those who do need daily monitoring.
This initiative offered a way to improve patient experience, maximize caregiver efficiencies, minimize radiation exposure and standardize practices with no negative impact on patient outcomes.
Dr. Reddy is Quality Officer in the Medical Intensive Care Unit and Associate Director of ICU Operations at Cleveland Clinic.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management