New developments offer providers more sophisticated options
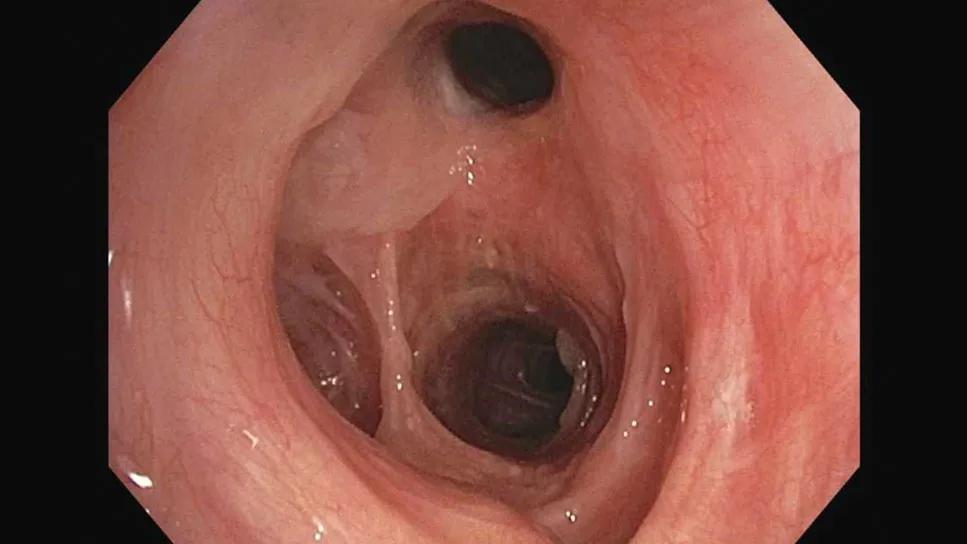
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a2537fcc-877c-439d-83ac-fa372460d8d1/airway-stent-scope)
Bronchoscopy showing silicone stent
Airway stenting has been used to help patients breathe for more than three decades, but there’s still great variability in how and when it’s used. This is partly due to a lack of research on the practice and variability of stent technology. Now, a new review by Cleveland Clinic physicians takes a closer look at stenting, the strengths and limitations of available stents, and the latest advances in the field.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Coauthor Thomas Gildea, MD, a Cleveland Clinic pulmonologist, says that while it’s clear stenting is a valuable tool for managing airway blockages, careful patient selection and management are key. New developments like 3D printing are addressing some concerns and giving providers more sophisticated options, but with a high complication rate, stenting should still only be used as a last resort.
“There’s a constant tension between putting a stent in because it makes the patient feel better or it makes the airway look better, and actual outcomes,” Dr. Gildea says. “It’s not always clear that the patient will clear, obvious long-term benefit from the device.”
Traditional options for stents include silicone stents. These devices are simple tubular structures that are available in a few different varieties and are relatively easy to insert and remove if done by an experienced provider.
However, these “old standbys” also have some limitations, including a propensity to mucus occlusion, says Dr. Gildea. In addition, as thick, rigid structures they are often a poor fit for the patient’s anatomy, making them prone to migrate.
A variety of metal stents are also in use, including laser cut and woven stents, with different coverings available. While these stents can be self-expanding and are more flexible, making them a popular choice for benign disease, they can still irritate the mucosa and cause other complications, Dr. Gildea explains.
“Although they’re better than prior generations for fit, they are still not perfect,” he says.
Advertisement
Enter 3D printing. These silicone devices retain the basic tube structure of traditional silcone stents, but they are customized to the shape of the patient’s anatomy. This allows for a more precise fit, reducing the potential for migration. Dr. Gildea explains that it also allows providers to design stents to fit areas of the anatomy where earlier stents could not be placed at all.
“There’s a whole world of difference between stents, and each of them has a role in different circumstances,” he says.
3D printed stents are currently in regular use at the Cleveland Clinic, and in addition to the advantage of customization, they can also be used to alter the patient’s prescription over time, such as adjusting the size of the stent to allow for a bigger airway as the patient’s inflammation subsides or using stents as a kind of “Invisalign for the lungs” to train the airway into a more normal shape.
“We’ve seen examples of a person who may have had severe airway inflammation and scarring, where we’ve placed a 3D printed stent, and over time the airway remodeled around the stent,” he says. “By altering the prescription repeatedly over time, we can get a better and often closer to normal airway.”
Looking ahead, there’s growing interest in incorporating novel materials in 3D-printed stents, such as bio-absorbable materials that dissolve in the body, or materials that incorporate therapeutics to prevent mucus blockage, infection or treat underlying disease.
Even with new tools and technology, an important concern in the world of stenting remains the high degree of variability, he said. Without clear, evidence-based guidelines, providers take wildly different approaches around such questions as the frequency of follow up visits after placing a stent, whether to use CT scans, symptoms or bronchoscopy for routine monitoring, the best way to manage mucus occlusion, and whether to use antibiotics prophylactically or only after infection occurs.
Advertisement
Dr. Gildea believes more research is needed to provide clarity around best practices. What is clear, he adds, is that patient selection is key for stenting. Given the high rate of complications with airway stents, providers should make their use contingent on seeing some kind of measurable improvement in the patient’s condition, whether that means reduced shortness of breath or improvement on a lung function test.
Patients should also be good candidates for managing and surviving potential complications, he notes.
“Because the complications are so common, and because the work of taking care of a stent can be so challenging, stenting should really be an option of last resort,” says Dr. Gildea.
The paper, “Advancements in airway stents: a comprehensive update,” was published in Current Opinion in Pulmonary Medicine.
Advertisement
Advertisement
Target levels of oxygen saturation might only be achieved around one-third of the day, according to available literature
Lessons learned from cohorting patients and standardizing care
Excessive dynamic airway collapse presenting as dyspnea and exercise intolerance in a 67-year-old
Despite a decline in numbers, the demand for respiratory therapists continues to rise
Quality improvement project addresses unplanned extubation
Staged pivotal noninferiority study is comparing BrioVAD with HeartMate 3
Study explores center volume and outcomes using the STS-Pedimacs database
Cleveland Clinic series supports its feasibility, especially with HeartMate 3