Dramatic improvements seen in adults with F508del mutation
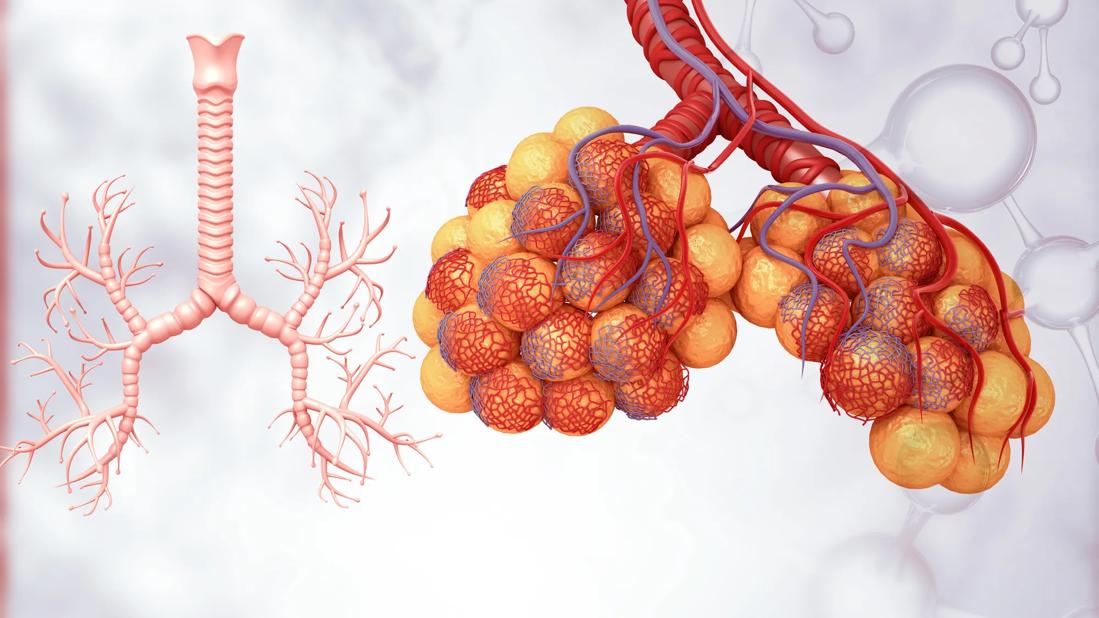
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c6d6cefc-c386-46f0-a2c3-f549e3060300/drug-changes)
Lung alveoli
Ninety percent of patients with cystic fibrosis (CF) have a mutation in F508del, and recently, treatment for them in Cleveland Clinic’s adult CF program has undergone a sea change. Use of elexacaftor/tezacaftor/ivacaftor and ivacaftor (TRIKAFTA) has become routine for this population, often leading to less mucus accumulation in their bodies, fewer trips to the hospital for exacerbations and better quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Because TRIKAFTA gets at the root cause of the disease, the clinical improvements have been tremendous,” says Elliott Dasenbrook, MD, Director of the Adult Cystic Fibrosis Program and the Bronchiectasis Center at Cleveland Clinic. “Particularly with the COVID-19 pandemic, it’s been a huge bonus for our patients to have less coughing and fewer acute flares of their CF requiring hospitalization.”
An oral agent, TRIKAFTA activates the CF transmembrane conductance regulator (CFTR), resulting in improved clearance of mucus in the airways, with clinical improvements sometimes seen within a couple of weeks. In October 2019, it received fast-track approval from the FDA for use in CF patients aged 12 and up with a F508del mutation, based on the very robust improvement in pulmonary function seen in two phase 3 trials.
In the first trial, patients who received the drug had a 13.8% absolute improvement in lung function from baseline vs. placebo, as measured by percent predicted forced expiratory volume in one second (ppFEV1). At week 24, TRIKAFTA treatment resulted in reductions of 63% for pulmonary exacerbations, 71% for hospitalization and 78% for IV antibiotic use. Sweat chloride was reduced by 41.8 mmol/L, and body mass index increased by 1.0 kg/m2, on average.
In similar patients in the second trial, which was double-blind, active-controlled and head-to-head, an increase in ppFEV1 of 10 percentage points was seen with TRIKAFTA and a 45.1 mmol/L reduction in sweat chloride levels at week four. Those results were in comparison with a control group who took tezacaftor/ivacaftor and ivacaftor. Patients on TRIKAFTA also had an improvement of 17.4 points on the Cystic Fibrosis Questionnaire Revised (CFQ-R) compared with those taking the active comparator.
Advertisement
Since TRIKAFTA became available, Dr. Dasenbrook has treated the vast majority of adults in the CF clinic with TRIKAFTA and has seen similar responses in many of them. The caveats are that individuals with elevated liver function tests require close monitoring while on the drug and that approximately 10% of CF patients who lack the F508del mutation are not candidates for it.
On average, adults with CF have one to two pulmonary exacerbations per year that may require an extended inpatient stay and administration of IV antibiotics through a peripherally inserted central catheter. In Dr. Dasenbrook’s experience, treatment with TRIKAFTA has largely eliminated those events. “A lot fewer of our CF patients need IV antibiotics, and it’s a big benefit for them to get back the two to four weeks of their life every year that they otherwise would have spent in the hospital.”
In patients with more advanced CF, according to Dr. Dasenbrook, improvements can be particularly dramatic. “The analogy I would make is that TRIKAFTA is to individuals with CF what insulin was to diabetics. Some of our patients on feeding tubes have gained so much weight that we’ve been able to remove the tubes. Ten patients being evaluated for lung transplant had so much improvement in their lung function after receiving TRIKAFTA that their lung transplant work-up was put on hold.”
Because TRIKAFTA targets the actual CFTR abnormality, it addresses the multisystem nature of CF rather than just symptoms. Sometimes thought of as affecting only the lungs, the thick mucus associated with the disease also builds up in the digestive tract and other parts of the body.
Advertisement
Studies of TRIKAFTA in various subpopulations with CF are underway and being planned, both at Cleveland Clinic and other institutions. Says Dr. Dasenbrook, “We are participating in a clinical trial of a once-daily formulation and will be publishing our experience with the drug in CF patients awaiting lung transplants and studying its use in patients who have already undergone lung transplantation.”
He also has some advice, based on his own experience, for pulmonologists practicing in the community who see adults with upper lobe bronchiectasis and have sinus or gastrointestinal symptoms suggestive of CF. “Test them for the F508del mutation. I’ve diagnosed adults in their 20s, 30s and 40s with CF, and treatment with TRIKAFTA has dramatically improved their lives.”
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program