25-year series of over 1,000 patients reveals good long-term palliation, esophageal preservation
Fifteen years following Heller myotomy for esophageal achalasia, over 80% of patients are free from reintervention, and the vast majority who need a reintervention can be taken care of with endoscopic procedures such as pneumatic dilation or peroral endoscopic myotomy (POEM).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So found a retrospective study of 1,010 patients treated with Heller myotomy for esophageal achalasia at Cleveland Clinic from 1995 to 2020, during which fewer than 2% required esophagectomy. The results were presented earlier this year at the 104th annual meeting of the American Association for Thoracic Surgery (AATS).
“Scarce long-term outcomes data have been published for this relatively rare surgery,” says senior investigator Siva Raja MD, PhD, Surgical Director of the Center for Esophageal Diseases at Cleveland Clinic. “As a result, there is no consensus on optimal follow-up, and clinicians have struggled to advise patients about their prospects beyond the first few postoperative years.”
Achalasia is a rare esophageal motility disorder involving the absence of esophageal peristalsis and a non-relaxing lower esophageal sphincter. Patients may have significant swallowing problems, regurgitation, chest pain and weight loss. “Although achalasia is not a malignant disease, the quality-of-life effects can be quite significant,” Dr. Raja notes.
For over a century, the classic treatment has been Heller myotomy to create a surgical division of the lower esophageal sphincter, facilitating passage of food out of the esophagus.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e22629b2-ad9d-4dbd-81a5-131c3df7c343/heller-myotomy-CQD)
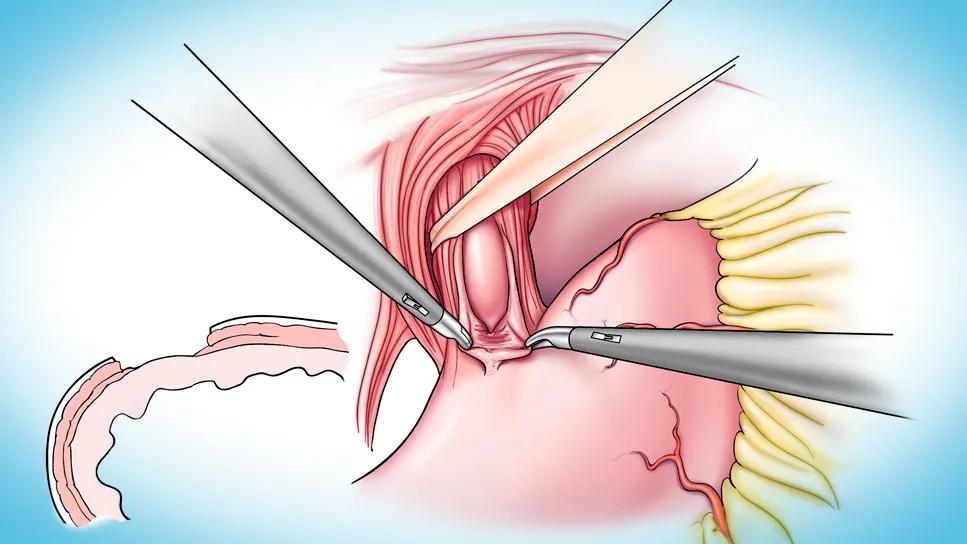
Illustration of a key step in the Heller myotomy procedure, which involves surgical division of the lower esophageal sphincter to facilitate passage of food. Here a bougie is passed to assist myotomy.
The methods have evolved over the years: originally performed with a thoracotomy, it is now often accomplished laparoscopically or robotically — and, more recently, endoscopically. Heller myotomy is usually accompanied by a Dor fundoplication, involving partial wrapping of the stomach around the esophagus to create a low-pressure valve to reduce reflux.
Advertisement
Despite the considerable experience surgeons have had with Heller myotomy, how the procedure relieves symptoms of achalasia is not completely understood. This study was designed not only to assess long-term symptom palliation and need for reintervention after the procedure, but also to analyze effects on esophageal emptying over time.
Across the cohort of 1,010 patients from 1995 to 2020, 74% of myotomies were performed laparoscopically and 19% with robotic assistance. “Robotic myotomy was used almost exclusively in the last five to six years of the study period,” Dr. Raja notes. Nearly all patients also underwent Dor fundoplication.
Patients were assessed annually for at least the first three years after myotomy, and every two to three years thereafter.
Over the course of the study, 187 reinterventions were performed in 134 patients, as follows:
Patients who underwent reintervention were at increased risk for a subsequent one: while 81% of the entire cohort was free from reintervention after 15 years, only 64% of those patients who underwent reintervention were free from a second reintervention 12 years after the first.
Follow-up monitoring included Eckardt scoring, which assigns a point value from 0 (never) to 3 (with each meal) for each of three symptom categories — dysphagia, chest pain and regurgitation — as well as for weight loss, where 0 denotes no weight loss and 3 indicates loss of more than 10 kg.
Advertisement
Conventionally, an Eckardt score ≤ 3 is considered successful. In this cohort, a score ≤ 3 was achieved in 93% of patients at one year and 73% at 10 years. Patients who eventually needed a future reintervention had higher scores early on.
“We could predict patients who required a future reintervention based on early appearance of symptoms,” Dr. Raja says. “The good news is that after we reintervened, these patients achieved Eckardt scores close to those of the overall group.”
He adds that while the presence of symptoms at the first preoperative visit does not provide good prognostic information, patients with persistent symptoms within the first two years need to be followed closely and considered for reintervention. Most reinterventions were needed in the first few years after myotomy.
Follow-up monitoring also included timed barium esophagogram (TBE), which involves measuring the height and width of the esophageal column with an X-ray at one and five minutes. The TBE was devised at Cleveland Clinic about 30 years ago specifically for patients with achalasia to indicate how quickly the esophagus empties.
“A normal esophagus empties in about 30 seconds,” Dr. Raja notes, “whereas a patient with achalasia may feel great even if it takes five minutes to completely empty, as it could have taken hours to days to empty prior to surgery.” Using five minutes as the standard, 56% of patients in the cohort achieved complete emptying immediately after myotomy, which gradually decreased to 24% at 10 years.
Advertisement
Interestingly, he adds, it was not necessary to have complete emptying to achieve excellent symptom relief. Few patients who required a future reintervention ever achieved complete emptying at five minutes. After reintervention, TBE improved only modestly, yet patients achieved good Eckardt scores.
“There is a discordance between how patients feel and how their esophagus behaves,” Dr. Raja says. “We still do not understand this adequately.”
In view of these findings, Dr. Raja recommends that patients have annual follow-up with Eckardt score assessment and TBE testing for the first three years after myotomy, after which the follow-up interval can be lengthened to every two to three years. “The risk of symptom recurrence and need for reintervention are greatest early on after myotomy,” he explains. He recommends endoscopic surveillance every five years in all patients on a lifelong basis, as well as in the wake of worsening symptoms or emptying.
Dr. Raja emphasizes that this large series demonstrates that Heller myotomy provides durable long-term palliation for esophageal achalasia, with the esophagus preserved in more than 98% of cases. “Regarding the role of newer endoscopic interventions for this indication, this is the bar that that must be met,” he concludes.
“This study not only demonstrates the long-term success in palliation with Heller myotomy, it also guides our surveillance for these patients after their surgery and our strategies for reintervention in case they need it,” adds Cleveland Clinic thoracic surgeon Monisha Sudarshan, MD. “For such a rare disease and infrequent surgery, these results will be vital in shaping our practice for patients with achalasia.”
Advertisement
Advertisement

Case highlights the benefits of a minimally invasive approach

3 pediatric gastroenterologists discuss advances in their diagnostic toolkits

Going beyond the Eckardt symptom score to evaluate dyspepsia, eating and symptom “bother”

Modified Barium Swallow Study and Flexible Endoscopic Evaluation of Swallowing can both be used to diagnose dysphagia, but it’s important to understand their advantages and disadvantages

Microvascular “supercharging” is a critical newer step to promote favorable outcomes

Research could help direct care pathways for patients with unexplained swallowing difficulties

Potential for new, non-invasive screening option

Pediatric and adult gastroenterologists offer team care for patients with eosinophilic esophagitis