Challenging an old surgical standard
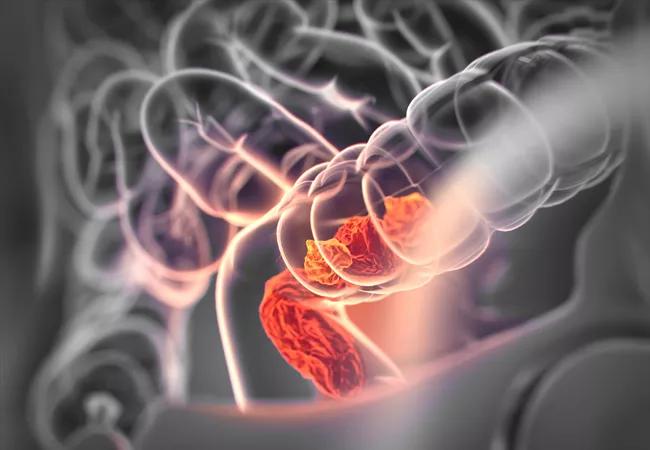
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b6b74979-0b5a-4106-89aa-1c27be6108f0/18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl_jpg)
18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl
The early removal of pelvic drains following abdominoperineal resection (APR) for rectal cancer is not associated with increased pelvic or perineal surgical site infections (SSI), according to a retrospective study presented at the American Society of Colon & Rectal Surgeons 2021 Annual Scientific Meeting. This finding challenges the longstanding surgical dogma that leaving pelvic drains helps prevent SSI or perineal wound complications after APR and encourages further prospective trials investigating the omission of pelvic drains following APR.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Recently, prospective trials have shown that pelvic drains are not helpful in the context of low anterior resection for rectal cancer,” says David Liska, MD, Director of the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia at Cleveland Clinic’s Digestive Disease & Surgery Institute and senior author of the study. “And yet, most surgeons still use them, hoping to reduce pelvic fluid collection and infection, or perineal wound complications but with no data supporting their use.”
Currently, timing of drain removal varies widely and is sometimes guided by arbitrary levels of drainage volume. Enhanced recovery protocols (ERP) call for avoiding drains or removing them early to accelerate recovery and patient discharge.
Researchers reviewed all rectal cancer patients treated with APR at Cleveland Clinic from 2009 to 2017 and tracked preoperative patient factors, operative details and 30-day outcomes. They separated patients whose pelvic drains were removed after volume decreased to < 150 mL and those with drain removal with output ≥ 150 mL.
Of 139 patients included, 53 had drain volume ≥ 150 mL on the day preceding removal, and 86 had removal following a volume decrease below < 150 mL. The high-volume removal group had pelvic drains removed earlier (median 4 days vs. 6 days, P < 0.001) than the group with lower drain volume upon removal. They also more frequently had minimally invasive surgery (69.8% vs. 31.4%, P < 0.001) and were more often treated within the context of an ERP (39.6% vs. 15.1%, P = 0.002).
Advertisement
The early drain removal group had lower overall morbidity (43.4% vs. 67.4%, P = 0.009) and incisional SSI (7.55% vs. 22.1%, P = 0.045). Researchers found no significant difference in pelvic and/or perineal SSI between the groups (11.3% vs. 22.1%, P = 0.168). When controlling for differences in the use of minimally invasive surgery and ERP, early drain removal was not associated with increased pelvic or perineal SSI.
“Instead, we found that delaying drain removal was actually associated with an increase in morbidity,” says Dr. Liska (RR = 1.48, P < 0.001).
These results are in line with findings of recent prospective trials that pelvic drains after low anterior resection for rectal cancer are not of benefit to the patient. “We demonstrated that removing the drains sooner, regardless of drainage volume, confers no disadvantage,” says Dr. Liska. “These findings lay the groundwork for future prospective trials and get us one step closer to deconstructing the surgical dogma of routinely using pelvic drains after abdominoperineal resections for patients with rectal cancer.”
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality