New study stratifies cardiac risk in radiation- and anthracycline-exposed patients
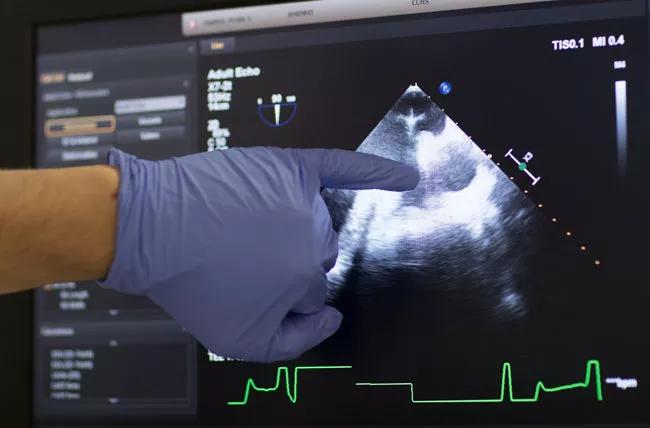
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0468222e-90c7-4981-a84e-7c57a9e6562c/18-HRT-311-Valley-Health-CQD-Hero-650x428_jpg)
18-HRT-311-Valley-Health-CQD-Hero-650×428
Cardiac injuries, particularly left ventricular systolic dysfunction, are a common consequence of hematopoietic stem cell transplantation (HSCT) during childhood and adolescence.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But guidelines and clinical protocols vary regarding the need, frequency and duration of post-transplant echocardiographic screening in long-term survivors.
New research by a team including Cleveland Clinic Children’s pediatric hematologist/oncologist Seth Rotz, MD, shows that HSCT survivors who are asymptomatic and didn’t undergo total-body irradiation or anthracycline-based chemotherapy are unlikely to have systolic dysfunction. As a result, these patients probably don’t need surveillance echocardiograms, unless otherwise indicated, after the first few years post-transplantation, the researchers conclude.
“This can result in savings of time and money for patients and the healthcare system,” Dr. Rotz says. “Patients often hear conflicting advice regarding heart health post-transplant. Hopefully this study can alleviate stress for some survivors.”
The retrospective study is the largest known examination of echocardiographic abnormalities in long-term pediatric HSCT survivors. It was conducted at Cincinnati Children’s Hospital Medical Center, where Dr. Rotz served his pediatric hematology/oncology fellowship.
Cardiac complications during and after HSCT are associated with a variety of etiologies: chemotherapy, medications, radiation, infection and transplant-associated thrombotic microangiopathy.
In previous research, rates of left ventricular systolic dysfunction in long-term pediatric HSCT survivors ranged from 0 to 26 percent. This large interval is due in part to inconsistent monitoring periods, varied methods to assess systolic function and differing risk factors among the populations studied.
Advertisement
Dr. Rotz and his colleagues sought to identify the rate of abnormal systolic function in survivors at least five years post-infusion, and to determine if a subset of survivors could safely avoid future echocardiographic screening.
The researchers reviewed echocardiograms and clinical data from surviving patients who underwent pediatric HSCT between 1982 and 2006 and received an echocardiogram at least five years after transplant. A total of 114 patients were identified; the 95 whose echocardiograms were performed for routine surveillance were compared to the remainder of the cohort, whose screenings were performed due to cardiac symptoms, congenital cardiac anomalies, hypertension, known cardiac or pulmonary disease, or unknown indications.
The researchers analyzed the echocardiograms for ejection fraction (EF — historically, the metric for left ventricle function) and left ventricular measurements, which they converted to age-adjusted z-scores.
The 10 patients in the study cohort whose EF z-scores were abnormally low (⩽−2.0) were significantly more likely to have been exposed to anthracyclines or total-body irradiation. Patients who underwent anthracycline chemotherapy had a mean z-score EF of -1.46 versus the mean z-score EF of -0.45 among patients who did not receive anthracyclines (p = 0.008). Patients who received total-body irradiation had a mean z-score EF of -1.79 versus -0.68 among patients who were not irradiated (p = 0.007). The positive predictive value of having an abnormal EF considering total-body irradiation or anthracycline exposure was 19.2 percent at 95 percent confidence interval (10.4-32.5 percent).
Advertisement
Of the 31 patients in the cohort who received neither anthracycline chemotherapy nor total-body irradiation, only one had an abnormal EF (z-score -2.73). This patient was asymptomatic.
“Our results demonstrate that long-term pediatric HSCT survivors who are asymptomatic and did not receive anthracyclines or irradiation were unlikely to experience abnormal ejection fraction or ventricular tissue deformation for at least 13 years post-transplant, which was the study’s mean,” Dr. Rotz says.
Currently, there are no cardiac screening guidelines for anthracycline/irradiation-naïve long-term HSCT survivors. The study shows these patients likely don’t need echocardiogram surveillance during the initial post-transplant decade unless otherwise indicated, Dr. Rotz says. Whether cardiac dysfunction will develop later in this patient population is unknown.
Conversely, pediatric HSCT patients exposed to anthracyclines or total-body irradiation appear at greater risk for systolic dysfunction and should undergo regular echocardiographic screening and clinical monitoring. Heart failure incidence is dose-dependent, and chemotherapy/irradiation effects may be subclinical and not detectable via echocardiography until cardiac reserves are depleted several years post-transplant, the study’s authors note.
Although this is the largest study to date in this patient population, a multi-center study of a larger population would validate these findings and could be incorporated into the next generation of guidelines, Dr. Rotz says.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches