Building the bridge between endocrinology and geriatrics

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/38410764-d122-44dc-8e44-e37baa7a702b/Endrocrine-Care-aging-stronger-better-1485021377)
endocrinology and geriatrics
As a dual specialist in endocrinology and geriatrics, Willy Marcos Valencia, MD, cares for patients with glucose and weight challenges as well as muscle or bone loss. His goal: Help them optimize their health so that aging means thriving rather than managing decline.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Valencia, who recently joined Cleveland Clinic with dual appointments in the Endocrinology & Metabolism Institute and the Center for Geriatric Medicine, believes in a comprehensive approach that extends beyond a given diagnosis or an isolated test result.
Endocrine problems such as obesity, diabetes, sarcopenia and osteoporosis, he says, are closely intertwined with mental, physical and social functions.
“They don’t start at any specific age, but they are clearly more prevalent in the older population,” Dr. Valencia says. “We must recognize we are all getting older. It’s just a matter of how we take care of ourselves and the conditions that impact our body. Time equals aging, but aging does not need to mean decline.”
Dr. Valencia advocates taking a broad view of the needs of these patients.
“The person is not just an A1C number, a bone density result, a weight or BMI number,” he says. “The patient is a whole individual, with multiple, connected, health-related domains. In addition to treating their endocrine conditions, I work on detecting, preventing and treating the geriatric syndromes of frailty, falls, depression, polypharmacy, functional and cognitive decline.”
Traditional doctor visits tend to focus on addressing specific issues, usually within a single medical domain. A geriatrics approach offers a panoramic view that also includes functional, mental and social domains.
“These domains are intertwined, and either they are impacted by the endocrine problems or they impact the ways we can treat them,” says Dr. Valencia. “They can also dictate the outcomes.”
Advertisement
His first research study on exercise was 18 years ago. Throughout his career, he implemented exercise programs that recruited thousands of patients for group exercise and individualized exercise prescriptions. He remains fascinated by the potential to improve people’s health with exercise.
“We know exercise works. We have tons of studies showing it,” says Dr. Valencia. “Not only does it improve metabolic and functional parameters, but also mental health conditions like depression and memory problems. The issue is that studies have an end, and often patient engagement also stops. We need to ensure lifelong commitment to these interventions.”
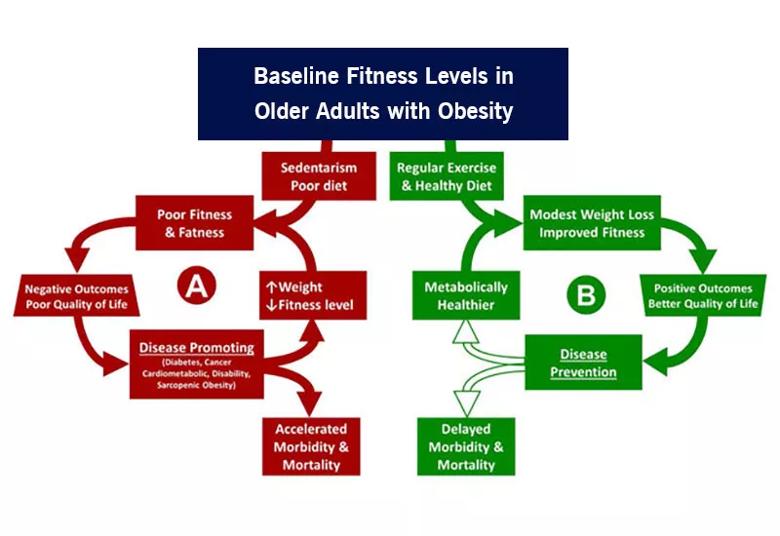
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e1cb9607-e0a5-4346-acde-c92c6f26e371/23-EMI-3533126-CQD-Inset-800x550-v2_jpg)
The negative cycle (a) indicates that poor fitness and overweight are followed by disease, disability and ultimately death. The positive cycle (b) shows how improved cardiorespiratory fitness, even with only modest weight loss, prevents disease and may prolong survival. Major events may interrupt the cycle, benefits often continue as long as regular exercise and a healthy diet are maintained.
In addition to exercise, proper nutrition is a key factor for aging success. Dr. Valencia discusses nutrition and protein intake with all his patients.
“I am convinced we must provide the resources — the protein — for those muscles to thrive,” he says. “My task at Cleveland Clinic is to build the bridge between Endocrinology and Geriatrics, and my first project is called Stronger, Faster, Better. I want to help patients improve their muscle strength and become stronger, and improve their gait speed and become faster.”
Advertisement
Patients should be guided to reach their protein intake targets, periodically adapt interventions to avoid complacency, and ensure ongoing improvements. Current and future technologies will help track and improve the monitoring of exercise and protein intake, he says. Technology will be used to measure body composition and enhance the understanding of improving health by doing exercise, forming muscle and losing fat tissue.
“Weight alone is not the only, nor the best, parameter,” says Dr. Valencia.
Patients who make changes that improve body composition can experience decreased polypharmacy, lower healthcare-related costs, and an increase in motivation to remain engaged with a lifelong commitment to better health, he says.
“Life will happen, and there might be life events that can set us back, but increased resilience helps patients get back on track,” says Dr. Valencia. “Our endocrine-geriatrics bridge aims to implement the clinical and research projects with long-term monitoring, to confirm these long-term successful results.”
Advertisement
Advertisement
Initiatives focus on the physical and emotional well-being of geriatric patients and their caregivers
Researchers explore the mental and physical benefits of social prescribing
Study suggests inconsistencies in the emergency department evaluation of geriatric patients
How providers can help prevent and address this under-reported form of abuse
How providers can help older adults protect their assets and personal agency
Early screening — and shorter boarding times — benefit older adults
Even subtle red flags can portend serious risks for older victims
Complications highlight need to exercise caution when managing geriatric patients