Study analyzes data from 60 per-oral pyloromyotomy cases
Using new technology and an advanced level of endoscopic expertise, physicians at Cleveland Clinic are offering a new technique to patients to treat gastroparesis, a common and often debilitating GI condition. Now a study confirms what many clinicians observed ― that per-oral pyloromyotomy (POP) could be a viable option for many of these patients with delayed gastric emptying who might otherwise undergo laparoscopic pyloroplasty.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Assessment of 60 people, half of who were treated with this endoscopic approach, revealed favorable outcomes that were comparable to many common surgical approaches, as reported in the journal Surgical Endoscopy.
“We picked up on the clinical effectiveness almost right away. I was not very surprised because we noticed patients coming back for follow up feeling better at the same rate that does undergoing pyloroplasty did,” says study co-author John H. Rodriguez, MD.
The researchers reported 86 percent of patients with gastroparesis undergoing POP and 83 percent who laparoscopic surgery showed improvement. This difference was not statistically significant.
Almost two-thirds, 63 percent, of the study population, presented with idiopathic gastroparesis. The remaining etiologies included post-surgical gastroparesis in 20 percent and a diabetes-related condition in 17 percent.
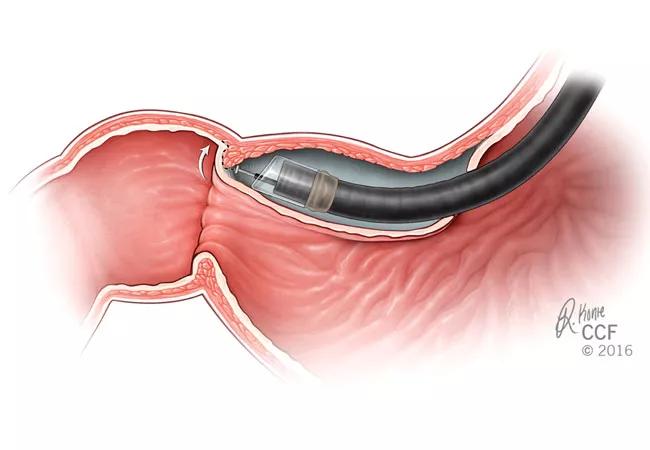
Patients with gastroparesis often experience nausea, vomiting, bloating and a feeling of early satiety. When medication therapy fails to significantly improve these symptoms, historically the next step is laparoscopic pyloroplasty, roux-en-y gastric bypass, gastric electrical stimulation or another surgical approach. With POP, endoscopic surgeons create a submucosal tunnel to approach and then divide the circular muscular fibers of the pylorus.
“The main advantages of POP include less invasiveness and a shorter recovery time,” Dr. Rodriguez says. In addition, recently he and fellow surgeons have performed the endoscopic technique on an outpatient basis, thereby helping patients avoid one or more nights of hospital admission after surgery.
Advertisement
Dr. Rodriguez, lead author and research fellow Joshua P. Landreneau, MD, and their colleagues report similar outcomes between groups, including no significant differences in emptying retention or mean percent retention based on scintigraphy at four hours.
Procedure time and other factors did significantly favor POP over laparoscopy, however. The average POP intervention took 34 minutes compared to 99 minutes for laparoscopic pyloroplasty. In addition, estimated blood loss in the POP cohort, 0.4 mL, was less than the 13 mL in the laparoscopy patients. Both these findings were statistically significant (P < 0.001). The average length of hospital stay again favored POP at 1.4 vs. 4.6 days (P = 0.003).
Dr. Rodriguez and colleagues also found a lower rate of complications associated with POP compared to laparoscopic pyloroplasty. Available 30-day follow-up data demonstrated, for example, an overall complication rate of 3 percent with POP versus 17 percent with laparoscopy. The difference did not reach statistical significance, however.
Complications included a superficial surgical site infection and unplanned ICU admissions in the surgical cohort. Two patients in the same cohort developed postoperative pneumonia. No surgical site leaks were reported in the study. One patient in each group underwent a repeat procedure within 30 days; the POP patient had a negative diagnostic laparoscopy for abdominal pain and the surgery patient had a jejunostomy tube placed for nutritional support.
Advertisement
“The main advantage we saw in clinic was that patients did not have the physical limitations that typically come from surgical recovery,” Dr. Rodriguez adds.
A multidisciplinary team at Cleveland Clinic typically evaluates all patients with suspected gastroparesis, including psychiatrists, gastroenterologists and nutrition specialists. “Gastroparesis patients are a very complex subset. They usually have other coexisting medical problems, nutritional deficiencies, psychological diseases that can develop from suffering from a chronic GI disorder, opioid addiction, etc.,” Dr. Rodriguez says. “By treating patients in a more universal way, we have demonstrated that good clinical results can be achieved.”
Cleveland Clinic endoscopic surgeons have performed more than 200 POP procedures to date.
Many patients with medication-resistant gastroparesis make appropriate candidates, Dr. Rodriguez says, “but especially those with extensive prior abdominal surgeries or a high risk medical profile.”
For endoscopic surgeons, the difficulty of adopting this procedure is highly dependent on the technical abilities of the operator, Dr. Rodriguez says. “For those that have good baseline endoscopic skills and are already performing advanced cases, then adopting POP is technically easy.”
“Overall, given the equivocal functional outcomes with fewer perioperative morbidity, this study demonstrates that POP should be considered as effective as pyloroplasty for the surgical management of gastroparesis with a trend towards a safer profile,” the researchers wrote.
Advertisement
Research efforts are ongoing. The investigators are working a randomized study to provide level I evidence of POP’s effectiveness for gastroparesis. Evaluating the role of POP as a first-line therapy in this population and tracking its long-term effectiveness are additional aims.
Advertisement
Advertisement

Retrospective study highlights psychosocial predictors of bariatric surgery outcomes

Greater awareness among young patients is needed

Combining RFA with stenting improves survival rates, reduces post-ERCP complications

Poor response may be due to different tumor biology

Study sheds light on distant metastasis rates between upfront surgery and Watch & Wait strategies

Findings help close the knowledge gap around VTE practice patterns

Nationwide research underscores the importance of individualized treatment

Potential for non-invasive methods to transform adult celiac disease diagnoses