Spine surgery through the nose
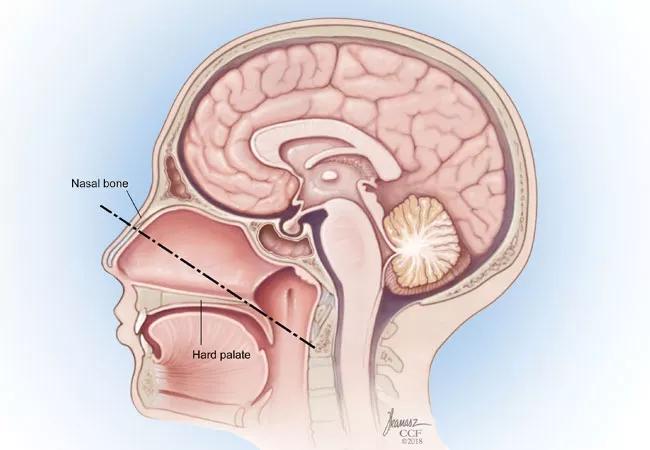
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/65e98ee5-5dcb-43fa-adcb-c86093af7bb9/18-ENT-4375-skullbase_650x450-002_jpg)
Figure 1 . The nasopalatine line, drawn from the inferior nasal bone to the posterior aspect of the hard palate and extended to the cervical spine, predicts the caudal extent of exposure for the endonasal approach.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By Raj Sindwani, MD, Christopher R. Roxbury, MD, and Zachary J. Cappello, MD
The craniovertebral junction (CVJ), which is composed of the occipital bone of the cranium and vertebrae C1 and C2, is an area through which many vital neurovascular structures, including the carotid and vertebral arteries, spinal cord and lower cranial nerves pass. Pathology in this region includes trauma, infections, inflammatory conditions and tumors, which may present with a variety of symptoms, such as neck pain, paresthesia, weakness, dysphagia and muscle spasticity.
This region has been notoriously challenging to access surgically, and the morbidity of open approaches has driven the development of minimally invasive approaches, initially through transoral routes, which require significant retraction or splitting of the soft palate.1 More recently, with the popularity of transnasal skull base techniques, an endoscopic endonasal approach to the CVJ, which provides direct access to this region while avoiding the morbidity of traditional open or transoral approaches has been developed.2
In preparation for surgery, patients are fused via a posterior cervical approach. This stabilizes the spine in anticipation of resection of the anterior arch of C1 and the odontoid process, which is the superior extension of C2. This allows rotation of the skull base about the cervical vertebrae. It can be done in a staged or sequential manner to the endoscopic endonasal procedure.
Once the spine has been rigidly fixed to prevent instability, our endoscopic skull base surgery team, which consists of a rhinologist working in tandem with a neurosurgeon, performs the procedure using technology that includes CT and MRI tracking surgical navigation. A two-surgeon, multi-handed technique is used to approach the craniocervical junction through a vertical incision in the midline of the nasopharynx. The limits of the surgical field are the basisphenoid superiorly, the paraclival carotid arteries and eustachian tubes laterally, and the nasopalatine line inferiorly (Figure 1-above image).3 Once the incision is performed with an extended needle-tip monopolar electrocautery, the dissection is carried through the pharyngeal constrictors, which are lateralized to expose the buccopharyngeal fascia. Sharp dissection is performed through the buccopharyngeal and preverterbral fascia to expose the anterior arch of C1.4
Advertisement
Once adequate exposure is obtained, the anterior arch is removed with a high-speed drill (Figure 2). Image-guidance is useful to confirm depth of dissection and orientation. Once the inner cortex of C1 is breached, the odontoid process is exposed. The superior ligamentous attachments of the odontoid are separated and the odontoid is removed with a combination of the drill and Kerrison Rongeurs. Depending on individual anatomy, removal of the inferior portion of the clivus can enhance superior exposure and facilitate the resection of the odontoid.4 Adequate decompression is accomplished when dural pulsations are noted at the posterior limit of the dissection, and care is taken to strictly avoid violation of the dura in order to prevent cerebrospinal fluid (CSF) leak.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e30b7f09-8a84-4b36-afe0-32d69c441edd/S-R-fig-2_jpg)
Figure 2. Visualization and drilling of the inferior clivus and anterior arch of C1 with lateralization of the nasopharyngeal mucosa and paraspinal musculature (or nasopharyngeal flap, NPF).
Once adequate resection of the odontoid process (Figure 3) and any related pannus or disease is achieved (Figure 4), the surgical field is examined for CSF leak with Valsalva maneuvers. As this is an extradural procedure during which a CSF leak should not be encountered — an involved reconstruction is not required. After hemostasis is obtained, the surgical wound is irrigated with saline and a small amount of absorbable hemostatic agent may be placed. The lateral aspects of the nasopharyngeal muscles and soft tissues are then approximated to the midline and the procedure is concluded.
Advertisement
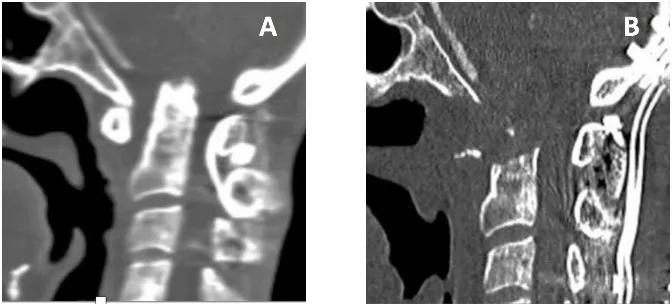
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/aa8ed6c7-19dd-492b-9e31-e6ef022b925f/S-R-fig-3_jpg)
Figure 3. (A) Preoperative imaging shows significant basilar impression and increased atlantodens interval with resultant severe narrowing of the spinal canal. (B) Postoperative imaging shows odontoidectomy and complete decompression. The arrow points to large odontoid process. Asterisk denotes resected area of the odontoid process.
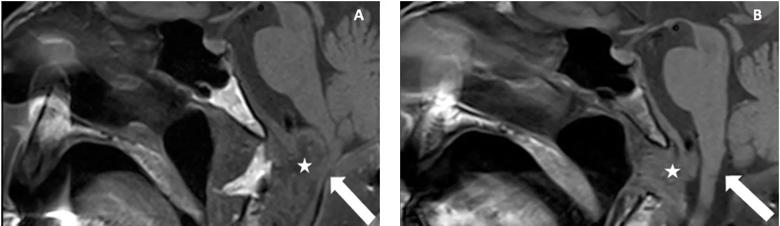
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/46c8f1f2-484c-4964-9b1d-db408384061a/S-R-fig-4_jpg)
Figure 4. A magnetic resonance imaging T1-weighted image in the sagittal plane. The asterisk indicates the pannus in (A) and reduced pannus and area of odontoid process resection in (B). The arrow is pointed to compressed portion of the spinal cord preoperatively and decompressed spinal cord postoperatively.
The endoscopic endonasal approach affords wide midline access to the CVJ and odontoid process, which respects the surgical tenet of not crossing major neurovascular structures. Namely, there is no need to retract or dissect the carotid arteries or lower cranial nerves. Therefore, there is potentially less risk for stroke and cranial neuropathies, which may result in dysphagia, dysarthria, and dysphonia. Moreover, the endonasal corridor avoids untoward effects of transoral/transpalatal approaches, such as wound contamination by oral flora, dysphagia and velopharyngeal insufficiency as a result of retraction or dissection of the soft palate.
Notably, the endoscopic endonasal approach also significantly reduces the need for tracheostomy postoperatively.5 In a recent review of the literature, it was found that only 3.4 percent of patients undergoing endoscopic endonasal approach for resection required a tracheostomy, which was significantly less than for the transoral approach.5
Advertisement
The endoscopic endonasal approach allows excellent access to pathology of the craniocervical junction, which was traditionally pursued through more invasive open or transoral approaches. This approach dramatically minimizes morbidity associated with open approaches and mitigates postoperative issues such as the need for tracheostomy, dysphagia and velopharyngeal insufficiency.
Dr. Cappello is the Advanced Rhinology and Endoscopic Skull Base Surgery Fellow in the Head & Neck Institute; Dr. Roxbury is rhinology and endoscopic skull base surgeon; Dr. Sindwani is Vice Chairman and Section Head of Rhinology in the Head & Neck Institute, and Vice Chair of Enterprise Surgical Operations for Cleveland Clinic.
1.Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and transnasal odontoidectomy complications: A systematic review and meta-analysis. Clinical Neurology and Neurosurgery. 148:121-129, 2016.
2. Alfieri A, Jho HD, Tschabitscher M. Endoscopic endonasal approach to the ventral cranio-cervical junction: Anatomical Study. Acta Neurochir 144:219-225, 2002.
3. De Almeida JR, Zanation AM, Snyderman CH, Carrau RL, Prevedello DM, Gardner PA, Kasam AB. Defining the nasopalatine line: the limit for endoscopic surgery of the spine. The Laryngoscope. 119:239-244, 2009.
4. Tang D, Roxbury C, D’Anza B, Kshettry V, Woodard T, Recinos P, Sindwani R. Technical notes on the endoscopic endonasal approach to the craniovertebral junction for odontoidectomy. Am J Rhinol Allergy. 2018 Mar;32(2):85-86.
Advertisement
5. Kshettry VR, Thorp BD, Shriver MF, Zanation AM, Woodard TD, Sindwani R, Recinos PF.Endoscopic Approaches to the Craniovertebral Junction. Otolaryngol Clin North Am. 2016 Feb;49(1):213-26.
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.