Insight on larynx disorders and treatments
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2241209/13920018)
Larynx disorders can significantly impact a person’s day-to-day life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
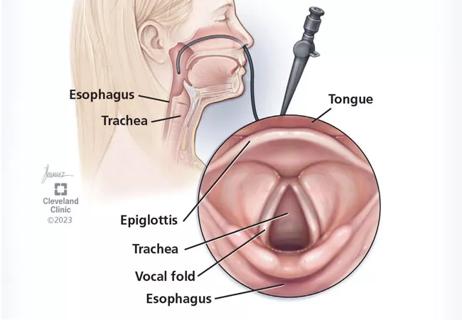
“Disorders of the larynx will encompass problems with the voice, airway or breathing and swallowing. So, it’s the things that we do every day – things that we take for granted,” says Rebecca Nelson, MD, a laryngologist at Cleveland Clinic. “And if you’re missing one piece of it, it can really affect your quality of life.”
In a recent episode of Cleveland Clinic’s Head and Neck Innovations podcast, Dr. Nelson shares insight on larynx disorders and treatments, including:
Click the podcast player above to listen to the episode now, or read on for a short edited excerpt. Check out more Head and Neck Innovations episodes at clevelandclinic.org/podcasts/head-and-neck-innovations or wherever you get your podcasts.
Podcast host Paul Bryson, MD, MBA: We had the opportunity to be co-authors on a paper called "Hoarseness, When to Observe and When to Refer," and that was published in our Cleveland Clinic Journal of Medicine. Do you want to share with the listener just a little bit about the paper and maybe make some points?
Dr. Nelson: Sure. So, this is kind of a highlight of the recently updated guidelines from our academy [the American Academy of Otolaryngology-Head and Neck Surgery] of when to refer, when observe. The take home points are if a patient comes in with hoarseness and they've had it for four weeks or longer, you really need to suspect something. It's not always something serious, but sometimes there can be a serious condition that's underlying, and they recommend actually expediting a laryngoscopy. So, get them referred over to an otolaryngologist or a laryngologist so we can scope them in clinic just to see what's going on.
Advertisement
There are a few different symptoms that can really suggest that there might be something going on – things like if the patient is an active smoker or has a significant tobacco history if they have a neck mass at the same time, that might indicate malignancy. But other things such as if they've been intubated recently. We're seeing some patients who have what's called a posterior glottic stenosis or an acute laryngeal injury from intubation, and they can have some pretty serious issues with their airway, sometimes voice-related to that. And so, getting them in sooner rather than later can make a difference in terms of outcome.
And then also things such as having recent head and neck surgery or chest surgery might indicate that they have a vocal cord paralysis that we can address. It's something that a patient doesn't need to suffer with for a long time. A lot of times we can get them in for a quick office procedure of vocal cord injection to get them to restore their voice sooner rather than later.
[The academy guidelines] also recommend avoiding just kind of treating it empirically with reflux medications, steroids or antibiotics. It's just really hard to know if it is an infection or something else just based on listening to their voice. And so, they're trying to avoid a kind of blind treatment of hoarseness.
If you can get a patient into our clinic, it's really easy for us just to take a look, and we can usually solidify a diagnosis right then and there. And that way we can really treat them with directed therapy that's going to help them rather than wasting time with the empiric treatment.
Advertisement
Advertisement

New innovations in upper airway care and insights into the Pediatric Voice Center
Cleveland Clinic physicians weigh in

A wide-ranging discussion on the latest in laryngology

A multidisciplinary approach and individualized plan of care are imperative

3 pediatric gastroenterologists discuss advances in their diagnostic toolkits

Injections and surgical procedures are among the therapies for patients with early and late vocal cord paralysis

A recently published case series highlights the broad range of laryngeal findings that can present among individuals with EDS

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor