New findings from a large retrospective study illustrate how understanding a patient’s pre-existing immune profile might impact COVID-19 outcomes
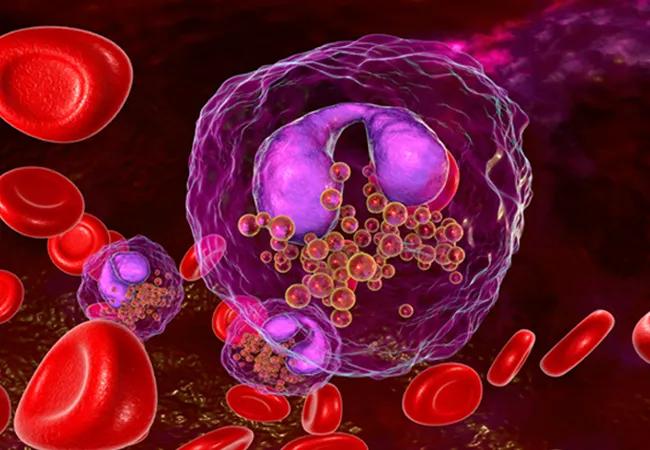
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a2a849a3-3dc6-4ffb-8f83-1213c9cbb0e0/21-PUL-2613965-CQD_Eosinophillia-Associated-with-Improved-COVID-19_650x450_jpg)
Eosinophil
Promising results from a new study indicate that pre-existing eosinophilia is associated with improved COVID-19 outcomes in inhaled corticosteroid (iCS) users. In non-users, the association between pre-existing blood eosinophil count and the probability of poor COVID-19 outcomes is non-linear (U shape). These new findings from a large COVID-19 Cleveland Clinic registry suggest that eosinophilia could be used as a biomarker to guide future randomized controlled trials evaluating the role of iCS therapy in COVID-19. The study appeared in The Journal of Allergy and Clinical Immunology: In Practice.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While eosinpohils are known to have anti-viral properties, much of the research on them is limited. Still, research suggests that eosinophils are associated with better outcomes among COVID-19 patients both with and without asthma. Along with high eosinophil counts, iCS have also been found to suppress COVID-19 with improved outcomes for patients by altering viral host interactions and their anti-inflammatory effects. But the effects of iCS on COVID-19-related outcomes in patients with asthma remains controversial.
Joe Zein, MD, PhD, a pulmonologist in Cleveland Clinic’s Respiratory Institute and the lead authors of the study explains, “We know that higher blood eosinophil counts have been associated with better COVID-19 outcomes in patients with asthma. But most of the data indicating this comes from epidemiologic studies that either relied on eosinophil counts obtained during the acute COVID-19 infection, have been limited to small sample size or did not account for the non-linear relationship between pre-existing eosinophil counts and COVID-19 outcomes. One of our objectives with this study was to study the effect of pre-existing immune profile on COVID-19 outcomes and determine if these earlier findings could be replicated with a much larger sample size.”
The present study tested the hypothesis that peripheral blood eosinophil counts influence risk for severe COVID-19 through interactions that are modulated by concurrent iCS therapy. The retrospective study analyzed data from the Cleveland Clinic COVID-19 Research Registry (April 1, 2020 to March 31, 2021). Of the 82,096 individuals who tested positive, 46,397 had blood differential cell counts obtained before SARS-CoV-2 testing dates. The endpoints included: hospitalization, admission to the intensive care unit (ICU) and in-hospital mortality.
Advertisement
Dr. Zein says, “Because of the wide range of outcomes patients with COVID-19 experience, it was obviously important for us to try to figure out how to better identify patients at risk for severe outcomes. To our knowledge, this is the first study to associate baseline immune cell profiles with the response to COVID-19 infection progressing to hospitalization, ICU care and death. We believe we are also the first to examine the impact of changes between baseline and peri-COVID-19 immune profiles on these severe outcomes.”
In the final analysis, the 46,397 patients were broken down as such: 19,506 had pre-existing eosinophilia (>0.15 x103 cells/μL), 5,011 received iCS, 9,096 (19.6%) were hospitalized, 2,129 (4.6%) required ICU admission and 1,402 (3.0%) died during index hospitalization. Patient demographics varied quite a bit, and the mean age was 56.3 years [IQR, 42.1; 69.3], and 10,609 (54.4%) were female.
Originally, the authors found that in regard to COVID-19-related outcomes, baseline eosinophilia had higher rates of hospitalization (21.2% vs. 18.4%, p<0.001), ICU admission (5% vs. 4.3%, p<0.001), and in-hospital mortality (3.4% vs. 2.7%, p<0.001) than those without pre-existing eosinophilia in unadjusted comparisons. However, after adjusting for demographics, BMI, smoking history, medications, comorbidities, the month of testing and the time between the absolute eosinophil count (AEC) test date and the COVID-19 test date, patients with eosinophilia (n=19,506) were actually at a significantly lower odds for hospitalization (adjusted OR [95 %CI]: 0.96 [0.93; 0.99]) and ICU admission (adjusted OR [95 %CI]: 0.92 [0.87; 0.98]) as compared to patients without eosinophilia (n=26,891).
Advertisement
One of the other major findings from the study is that the association between COVID-19-related outcomes (hospitalization, ICU admittance or mortality) and baseline AEC is nonlinear, and it varies according to iCS use. The predicted probability for COVID-19-related outcomes was higher among individuals with elevated AEC who had not been treated with iCS as compare to those with normal AEC. This association was not seen among iCS-treated patients. The authors believe these findings suggest that iCS somehow modulate disease severity for those with high but not low eosinophil counts.
“Our findings suggest that the risk of severe COVID-19 is highest among individuals with eosinopenia irrespective of iCS therapy,” says Dr. Zein. “So if future studies are able to corroborate our findings and assess the effect of eosinophilia on the hyper-inflammatory state seen in severe COVID-19, then we can use eosinophilia as a biomarker to guide future randomized controlled trials evaluating iCS therapy in COVID-19.”
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program