Shorter esophagus often means recurrence
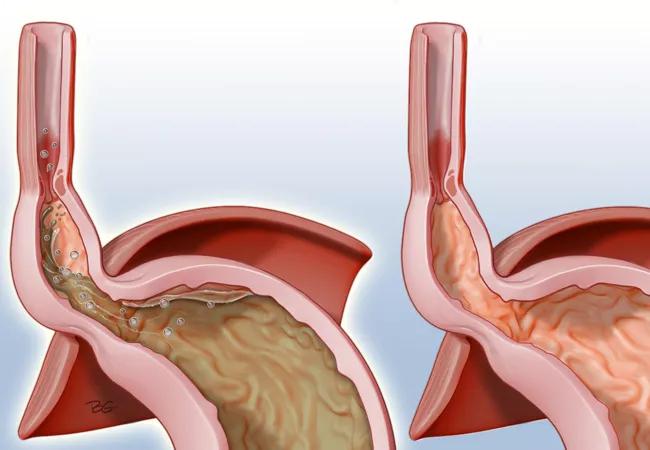
The first line of treatment for patients with a hiatal hernia is Nissen fundoplication, a surgical procedure — often performed laparoscopically — in which the top of the stomach is wrapped around the lower esophagus to hold it down below the diaphragm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sometimes, however, this procedure fails. Patients experience recurrence of the hiatal hernia and may need a different surgical intervention such as Collis gastroplasty, in which the esophagus is lengthened through an incision in the stomach and then the stomach is wrapped around this neo-esophagus. Collis gastroplasty must be performed as an open surgery so it is riskier than laparoscopic Nissen fundoplication.
Predicting which patients may experience hernia recurrence after surgical intervention was the goal of a recent retrospective study performed by gastroenterologists at Cleveland Clinic. The researchers wondered whether esophageal length — which is usually measured prior to surgery via manometry — might predict such recurrence.
“It’s a variable that’s available to all patients, but no one has really paid attention to it as a predictor of surgical outcomes,” says gastroenterologist and hepatologist Scott Gabbard, MD. Dr. Gabbard recently presented the results of this study today at the American College of Gastroenterology 2018 Annual Scientific Meeting.
The researchers looked at medical records of 274 patients who underwent pre-operative esophageal manometry and either open or laparoscopic primary hiatal hernia repair between 2005 and 2015.
To control for difference in body type, the researchers divided the length of patients’ esophagi by their heights. “Because clearly someone who is 4 foot 6 should have a shorter esophagus than someone who is 6 foot 6,” says Dr. Gabbard.
Advertisement
The researchers found the patients had an esophageal length-to-height ratio that ranged between 0.1 and 0.15. Those with a ratio of 0.12 or lower had dramatically increased rate of hiatus hernia recurrence, says Dr. Gabbard. The data also showed that 68 of the patients, 24.8 percent, had hernia recurrence and that Collis gastroplasty decreased hernia recurrence by 80 percent.
“The purpose of the study was to try and predict which patients would be most helped by the more the invasive Collis gastroplasty versus the less invasive laparoscopic fundoplication,” explains Dr. Gabbard. “Our data would suggest that Collis gastropolsty should be strongly considered for any patient who has an esophageal length-to-body height ratio of less than 0.12.”
The information is important for gastroenterologists to be aware of because not all surgeons can perform both procedures, Dr. Gabbard says. “I’m using this ratio with my patients now,” he said. “It’s helping me to plan which surgeons to send them to.”
He and his colleagues plan to track their data going forward to see if this preoperative stratification through esophageal length-to-height ratio helps prevent a need for revision surgery.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years