Melanoma may be more heritable than we think

Pauline Funchain, MD, has a hunch that hereditary melanoma is more common than currently understood, and she’s leading the charge to learn more by establishing a new registry for families with unusually high rates of the cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Gross Family Melanoma Registry is an open-ended project that will start with about 100 patients and family members with high rates of melanoma. This initial cohort will undergo targeted evaluation with a 12-gene melanoma-specific panel test with an option to expand to a larger 80-gene pan-cancer panel test.
As patterns emerge, and depending on individual results, the protocol allows for further increase in scope to include whole exome or whole genome for perplexing familial cases where no notable patterns of heritability or genetic predisposition emerge during panel tests.
“Some research shows that 1 to 2 percent of melanoma cases are inherited,” says Dr. Funchain, associate staff in the Department of Hematology and Medical Oncology. “Among my patients, I see several each week with melanoma that has some kind of familial connection. When you add that up, the number is significant. I would estimate anywhere from 10 to 20 percent.”
Furthermore, evidence is mounting to suggest correlations between melanoma and susceptibility to other cancers, including prostate (in men), breast (in women) and non-Hodgkin’s lymphoma (in both). However, evidence on the reasons behind these correlations remains inconclusive.
Dr. Funchain believes at least some of the answers may lie in genetic patterns and predispositions that have yet to be discovered, and she intends to leverage the statistical power of the new registry to expose them.
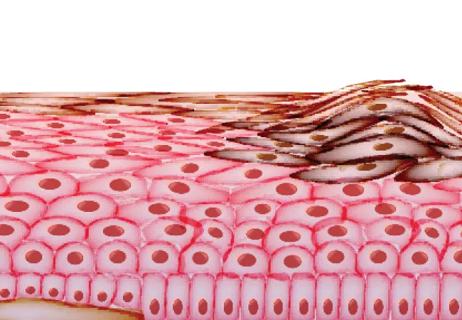
In terms of heritability, emerging research is showing that a person’s susceptibility to melanoma may have more foundation in their genes than any other cancer type.
Advertisement
For example, a recent study following 203,691 pairs of twins over 32 years across four Nordic countries found that melanoma had the highest familial component of any cancer evaluated. Results ranked the following cancers by percentage of cases attributable to inherited traits: melanoma (58 percent), prostate (57 percent), nonmelanoma skin (43 percent), ovarian (39 percent), kidney (38 percent), breast (31 percent), and uterine (27 percent).
“A lot of research is telling us that cancer is more familial than previously understood, but we’re behind on melanoma,” says Dr. Funchain. “If you compare what we know about melanoma versus what we know about breast cancer and colon cancer, there’s a big gap.”
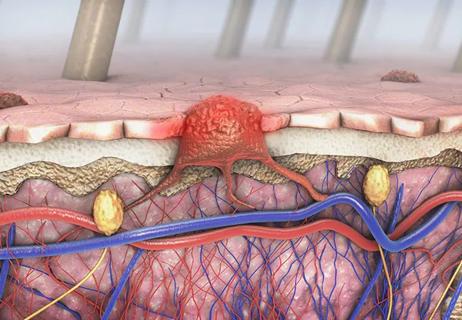
If a diagnosis of cancer is frightening for patients, news that an entire family is at greater risk can be terrifying — particularly when physicians have insufficient information to provide a satisfactory rationale.
“Anecdotally, many oncologists, including me, have cared for patients and families that have high rates of cancer, but all panel testing has come back negative,” says Dr. Funchain. “It’s incredibly frustrating for families, who feel powerless over the mystery of their melanoma risk.”
Participation in the registry not only will bolster understanding of melanoma heritability and genetic underpinnings; it also offers patients the option to learn test results, which they can share with family members.
“A lot of studies say, ‘Give us your blood, and we’ll take it into the lab to do some research, and we’re sorry but you’re never going to hear about it,’” says Dr. Funchain. “One of the really exciting components of this project is that we have the opportunity to do the research and give back to our patients at the same time.”
Advertisement
Identifying familial cancers represents an opportunity to pinpoint high-risk individuals who have not yet developed cancer, as well as identify people with a melanoma diagnosis who might be at risk for developing additional cancers.
“We’ve seen some data that suggests you really can save lives,” says Dr. Funchain. “You’re going to get colonoscopies earlier and get those precancerous polyps out before they become cancer. You’re going to have your ovaries removed before they become cancerous.”
“You literally can save family members’ lives, and that’s how we hope referring physicians and study participants see this, because the reality is that we’re not giving people a burden of knowledge — we’re giving them power to focus on prevention for themselves and their families.”
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Neoadjuvant immunotherapy improves outcomes

Largest study of its kind identifies three treatment exposures that contribute to risk

Family history may eclipse sun exposure in some cases
Immunotherapy is preferred initial treatment for majority of patients
Timing of adjuvant immunotherapy unclear for maximum overall survival

Highly personalized treatment shrinks tumors resistant to immunotherapy

Cleveland Clinic Cancer Institute among select group of centers to administer highly personalized treatment