Research demonstrates improved overall survival for patients receiving comprehensive treatment for breast cancer in addition to radiation or surgical intervention for brain cancer

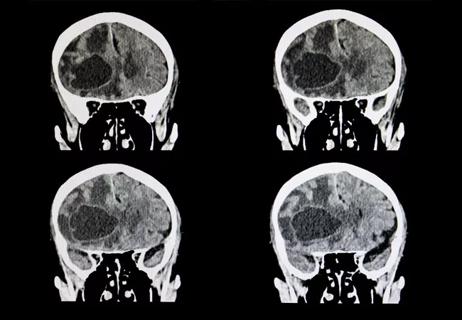
Although much progress has been made in treating breast cancer in recent years, addressing disease that has spread to the brain remains an unmet need. Historically, patients with breast cancer that has metastasized to the brain (BCBM) have poor outcomes. In order to focus treatment planning for these patients, a team of researchers conducted a large retrospective study to better understand the identifying factors and interventions impacting survival in patients with de novo BCBM.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The analysis suggests that treatment of systemic disease is a major factor influencing survival in patients with BCBM,” says Zeina Nahleh, MD, Cancer Center Director and Regional Chair of Hematology-Oncology at Cleveland Clinic Florida. “These findings highlight the importance of incorporating systemic treatment for the breast cancer itself and not just local treatment for brain lesions. Moreover, targeted therapy such as with anti-HER2 therapy increased survival when appropriately added to systemic therapy for certain subtypes of breast cancer.”
For the study, the researchers focused on patients who were initially diagnosed with breast cancer and de novo brain metastasis. “We wanted to understand what is significant about these patients and what could improve their treatment outcome,” says Dr. Nahleh.
The team analyzed National Cancer Database records of patients treated between 2010 and 2020. Out of 2,610,598 patients, 34% had de novo BCBM. The team considered characteristics of the de novo BCM group, including age, demographics, ethnicity, grade, type and more, across different treatment modalities.
Median overall survival was calculated using Kaplan-Meier curves and log rank tests. The team then applied a multivariate Cox regression model to identify predictors of survival.
The data revealed that the number of extracranial metastatic sites, increased age, comorbidities and Charles-Deyo score all correlated with decreased overall survival. Patients with the breast cancer subtype known as triple positive disease had the highest median overall survival, while triple negative patients had the lowest overall survival. Those patients receiving therapy targeted at specific mutations, along with systemic therapy, such as anti-HER2 treatment, experienced the best prognosis. Patients who were treated at an academic center fared better than those who received treatment at a community hospital setting.
Advertisement
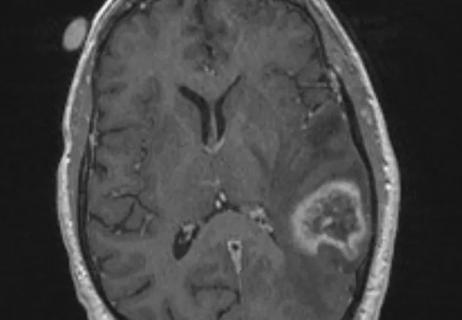
“Knowing the subtype of breast cancer is essential so we can tailor treatment accordingly,” says Dr. Nahleh. “We can’t treat all breast cancer the same way. Patients with triple-positive breast cancer actually do have a reasonably good prognosis if they’re treated with targeted therapy in combination with chemotherapy and brain radiation, hormonal therapy, and in some cases surgery on the brain.”
Through their analysis, the researchers found there were some patients who did not receive systemic therapy for one reason or another. In some cases, patients received local treatment of the brain instead of the full body. “Those patients had inferior outcomes,” says Dr. Nahleh. “The takeaway is that treating breast cancer in a comprehensive manner instead of just focusing solely on the local brain lesions can make a big difference in outcomes.”
This study further validates the point that breast cancer is not one disease. Breast cancer is a heterogeneous disease. Patients with triple positive, hormone-positive or HER2-positive breast cancer – even with brain metastasis – can have a good outcome with appropriate treatment. “There may be a tendency to feel discouraged and like you can’t do anything because of brain metastasis, but these study findings are a call to treat patients with de Novo brain metastasis more aggressively if they can tolerate treatment, particularly in those subtypes that tend to fare better,” says Dr. Nahleh. More research is needed to improve the outcome of BCBM and promising novel agents are being developed. “The right combination of therapy and the advances in precision therapy can make a tremendous difference.”
Advertisement
Building on this research, Cleveland Clinic Main Campus and Cleveland Clinic Weston, FL are creating a database to follow patients with brain metastasis, recording data such as the patient’s performance status, number and size of brain lesions, type of chemotherapy or targeted therapy and/or surgical interventions, radiation dose and more. This will enable researchers to analyze more data points to better understand appropriate interventions that can improve outcomes.
Advertisement
Advertisement

Largest study to date comparing direct-acting oral anticoagulants to low-molecular-weight heparin

Improvements enable targeting of brain tumors with single-session, fractionated or neoadjuvant approaches
This approach led to local control for patients with brain metastases more than 2 cm in diameter
We now have an expanded toolbox to extend survival and lessen treatment toxicity

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Large retrospective study suggests DOACs are safe, effective alternative to low-molecular-weight heparin in complex patient population

Advances in genomics, spinal fluid analysis, wearable-based patient monitoring and more

Reconsidering axillary lymph node dissection as well as depth of surgical margins