New course highlights role of imaging in the diagnosis and management in TOF
The use of fetal echocardiography to guide management of congenital heart disease (CHD) in a setting of multidisciplinary care optimizes neonatal outcomes, according to Cleveland Clinic fetal cardiologist Rashmi Rao, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Rao, Associate Director of Fetal Cardiology, spoke during a Continuing Medical Education live course on the role of imaging in the continuum of care in tetralogy of Fallot.
“Fetal echocardiography offers important information for delivery planning. If we’re concerned that the baby will need any kind of therapy or surgery soon after birth, then we can help families prepare for delivery in our main campus special delivery unit,” says Dr. Rao, who is also Co-director of Cardiac Neurodevelopment and Psychosocial Well Being at Cleveland Clinic Children’s.
Indications for fetal echocardiography include maternal factors such as diabetes, autoimmune disease, or certain medications, a family history of structural heart defect, and/or fetal factors detected on obstetric ultrasound.
A major watershed in the field occurred in 2013, when obstetric ultrasound guidelines were expanded from a four-chamber view to also include assessment of the outflow tracts and three-vessel view. Adding these views has been shown to increase the sensitivity of screening programs to achieve a detection rate of up to 90% in some centers.
“Before 2013, routine obstetric ultrasound was missing many cases of congenital heart disease. When protocols were expanded to look at the fetal heart in more detail, they started identifying more congenital heart defects,” Dr. Rao notes.
Once a defect is identified, referral for fetal echocardiography is the next step. The modality provides critical information for planning the mode, timing, and location of delivery, and for anticipating initiation of prostaglandin and other postnatal interventions. The findings also can point to the need for genetic testing and counseling, and to implications for future pregnancies.
Advertisement
Dr. Rao presented two illustrative cases of the use of fetal echocardiography in tetralogy of Fallot (ToF), the most common cause of cyanotic heart disease. The prenatal detection rate of the condition has risen from 20% to 30% prior to 2014 to 50% to 60% today with cardiac screening.
In ToF with mild-to-moderate pulmonary stenosis, aka “pink tet,” the fetal echo demonstrates some obstruction in the flow across the pulmonary valve, but still with sufficient flow to the lungs that there would be no immediate need for intervention. Here, the management involves ongoing fetal cardiology follow-up, amniocentesis and genetic testing, and plans for postnatal monitoring.
“We still have them all deliver on Cleveland Clinic main campus unless there’s no level of obstruction of flow to the lungs and observe them in the hospital, but we can counsel the parents that they should be able to go home and come back later for the surgical repair, usually in about four to six months,” Dr. Rao explains.
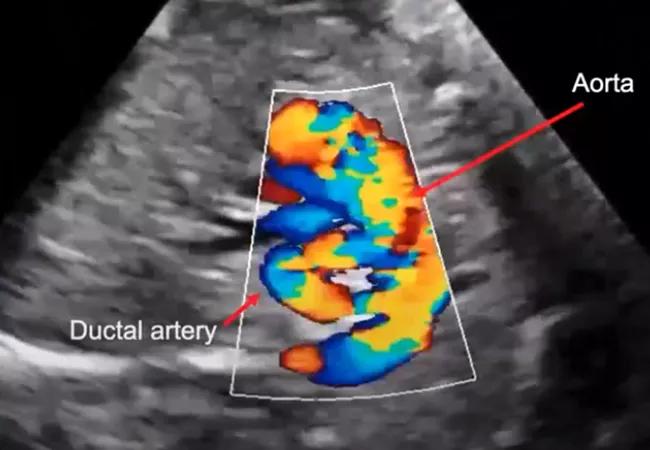
However, echo-informed planned management is far different in a case of ToF with pulmonary atresia, or “blue tet,” in which there is no visible anterograde flow from the right ventricle. This condition is much more severe, with no valve outlet or blood flow to the lungs. This baby must be delivered at the main campus and started on prostaglandin right away to keep the ductus arteriosus open until surgery, usually within a week to 10 days after birth.
Here, the use of fetal echo makes a major difference. “If we know about it and plan for it appropriately, we prevent a potential emergency,” Dr. Rao notes.
Advertisement
Indeed, data for other CHDs suggest that prenatal diagnosis via fetal echocardiography improves CHD outcomes by shifting intervention to earlier timeframes. Particularly with dextro-transposition of the great arteries and hypoplastic left heart syndrome, the result is reduced ongoing cardiac and neurologic impairment due to persistent hypoxia or unfavorable hemodynamics.
Prenatal diagnosis has also been linked to lower rates of major preoperative risk factors, such as shock and metabolic acidosis, and decreased use of mechanical ventilation and antibiotics. Several studies have shown that infants with prenatally diagnosed major CHD have better early and late neurodevelopmental outcomes.
Coordination of care is essential to this process. At Cleveland Clinic, all the relevant specialists – from OB/GYN to maternal-fetal medicine to fetal cardiology – are housed in the same center with shared medical records. Comprehensive consultations can all occur in one clinic visit.
“That’s pretty unique and not my experience elsewhere. Often, there are independent practitioners, not all working together, which requires a lot more coordination of care to ensure the best outcome,” Dr. Rao says.
In contrast, at Cleveland Clinic the relevant specialists hold weekly meetings to review care and delivery plans together. Other team members as needed include genetic counselors, psychologists, and pediatric specialists as the child transitions to post-surgical care. Concludes Dr. Rao, “We do everything we can to make the process as seamless as possible.”
Advertisement
Advertisement

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve

Reproducible technique uses native recipient tissue, avoiding risks of complex baffles

A reliable and reproducible alternative to conventional reimplantation and coronary unroofing

Program will support family-centered congenital heart disease care and staff educational opportunities

Case provides proof of concept, prevents need for future heart transplant

Pre and post-surgical CEEG in infants undergoing congenital heart surgery offers the potential for minimizing long-term neurodevelopmental injury

Science advisory examines challenges, ethical considerations and future directions