Panel proposes staging and treatment protocols that support harmonized evaluation and management of heart failure in patients with congenital heart disease

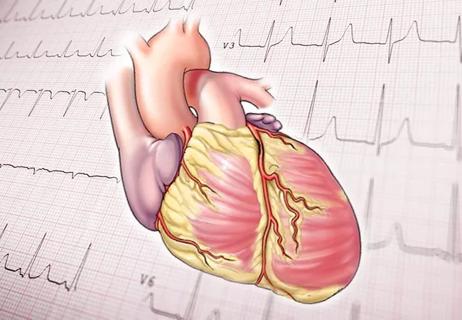
Most children with congenital heart disease (CHD) now survive into adulthood, making diagnosing and managing chronic heart failure (HF) in them a growing concern. To improve outcomes for these patients, clinicians must adopt harmonized definitions of chronic HF and approaches to staging, follow-up and treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those are the key takeaways from a new scientific statement from the American Heart Association on evaluation and management of chronic HF in children and adolescents with CHD, according to Shahnawaz Amdani, MD, Section Head of Pediatric Heart Function and Transplant at Cleveland Clinic. Dr. Amdani was chair and lead author of the document, recently published in Circulation.
“We’re seeing an avalanche of chronic HF in pediatric patients with CHD, and the healthcare community needs to be cognizant of that,” says Dr. Amdani. “This document represents an attempt by a panel of experts to inform clinicians on how to evaluate and manage these individuals, based on the limited available evidence.”
The scientific statement presents an overview of current epidemiology, pathophysiology, staging and treatment of chronic HF in children and adolescents with CHD who are not candidates for catheter-based or surgical interventions.
Studies indicate that up to 40% of children who undergo surgery for CHD experience chronic HF within 20 years after the procedure. Outcomes are the worst in those with single ventricle CHD, advanced heart failure symptoms and those with elevated cardiac biomarkers such as NT pro BNP and Troponin T.
In a list of 10 things to know about its statement, the panel notes that the etiology of chronic HF in CHD patients may be a result of chronic myocardial stress from underlying CHD physiology or injury to the myocardium. Genetic predisposition to cardiomyopathy also may play a role.
Advertisement
Says Dr. Amdani, “Ejection fraction-based categorization of ventricular dysfunction is standardized in adults with structurally normal hearts, but no such cut-offs have been developed for children and adolescents with CHD.” To fill that gap, the panel proposes a 3-level categorization of dysfunction in those with systemic left ventricular morphology:
Until better data are available for this with systemic right ventricle (RV), the experts recommend defining RV dysfunction based on an RV ejection fraction < 40% on cardiac magnetic resonance imaging or more than moderately depressed RV function on echocardiography.
A 4-stage framework for heart failure – from none through mild, moderate and severe – is proposed to characterize severity of HF in children with CHD and chronic HF. Yardsticks recommended by the panel include assessment of heart failure class; growth percentile; natriuretic peptides; myocardial oxygen consumption (MVO2) on metabolic exercise stress test; cardiac index and ventricular end diastolic pressure obtained by cardiac catheterization and evaluation of heart failure hospitalizations in the previous year.
“Any one of the factors or a combination of them can be used as a sensitive way of judging HF severity, which can change with therapy,” says Dr. Amdani. “No standardized scales exist for measuring HF severity in children and adolescents with CHD, so we hope this tool will help standardize assessment clinically and serve as an important tool for research studies.”
Advertisement
The panel also recommends that clinicians view stages of HF in pediatric patients with CHD akin to the adult HF classification. These stages have been tailored to be applicable to CHD patients. They encourage going beyond ventricular function and taking into consideration conduction system abnormalities and risk factors such as obesity, hypertension, diabetes, and exposure to cardiotoxic agents when assessing risk for HF.
Before instituting medical therapy for pediatric patients with CHD, the experts urge clinicians to evaluate and tackle any residual lesions. Measures to improve nutrition, address cardiac comorbidities, ameliorate anemia, and promote exercise and mental health also should be pursued.
Few data exist to support the safety and efficacy of prescribing for children and adolescents HF therapies that are recommended in guidelines for use in adults. Only enalapril and carvedilol have been studied in randomized clinical trials (RCTs) in children with CHD to date, and as noted by the panel, neither of the drugs showed a benefit for patients with subaortic right or single ventricular anatomy.
“Performing prospective RCTs in children with CHD and chronic HF is difficult because diagnoses in them are heterogenous, sample sizes and frequency of clinical events is small,” says Dr. Amdani. “To generate the high-quality data needed to advance and optimize therapy in this area, partnerships are needed among researchers, healthcare professionals, patients, caregivers and public and private funding agencies.”
Advertisement
Advertisement

Experts are challenging the one-size-fits-all paradigm

Decongestion, therapy titration and readmission rates comparable to those with traditional hospital care

Metabolites from animal product substrates implicated in heart failure development in community cohorts

Eminent clinician-researcher brings special expertise in nutritional interventions for heart failure

Recent volume and outcomes data in two major realms of cardiovascular care

Volatile organic compounds have potential in heart failure diagnostics

Basic understanding of condition and treatment is lacking
Indications and issues concerning cardiac resynchronization therapy, conduction system pacing