Study examines data and clinical implications for performing Ross procedures in infancy versus later in life
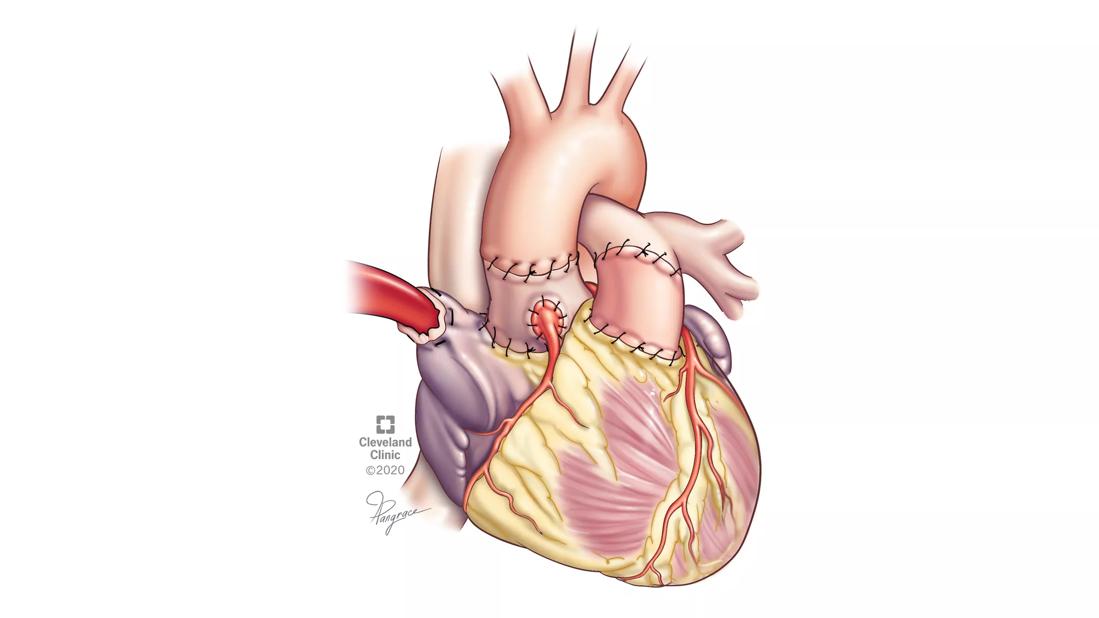
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/68467345-247f-4663-b6d2-59612022a6b8/ROSS_finish-5_2000066880_20-PAI-1977090)
Illustration of heart after Ross procedure
Determining the optimal timing to perform the Ross procedure on a child with aortic valve disease is a clinical conundrum. In a new paper, a team of experts reviews all the available data and lays out the pros and cons of performing it in infancy versus later in life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Ross operation involves the removal of the diseased aortic valve and replacing it with the patient’s own pulmonary valve (autograft), which, in turn, is replaced by a donor valve. Compared with mechanical valve replacement, the Ross avoids the need for blood thinners and, if done in infancy, allows for growth of the valve as the child grows.
However, neonatal mortality of up to 30% with the Ross has been reported across centers, considerably higher than in older children. Some experts also believe it is more advantageous instead to perform aortic valve repair in infancy and postpone the Ross until later in life when the autograft can be stabilized at an adult size and a larger right ventricle-to-pulmonary artery conduit can be placed.
“The Ross procedure is sometimes the best thing to do for growing children because we don’t have a small prosthesis that can fit them. But, if done very early in life, the mortality is relatively high. For that reason, some argue that we should just repair the valve to buy some time and then do the Ross later. But there are some surgeons who say that’s where technical expertise comes in,” explains Cleveland Clinic pediatric cardiac surgeon Hani K. Najm, MD.
Dr. Najm was among the 13-member expert writing panel from the U.S. and Canada who authored an “invited expert review” summarizing currently available data. Their aim is to provide surgeons a full look at all the considerations that should go into the decision for an individual patient rather than actual guidelines, since data are insufficient for that.
Advertisement
The authors list the following clinical implications:
1. Low mortality and good long-term outcomes for both aortic valve repair and Ross operation have been reported and can be achieved at centers with significant expertise.
2. Direct comparison of Ross operation and aortic valve repair in identical groups of patients is not possible currently, because the Ross procedure is typically performed in newborns and infants who have significant other cardiovascular anomalies or after failed balloon aortic valvuloplasty rather than isolated aortic stenosis.
3. It is possible that if Ross or Ross-Konno operation, in which the left ventricular outflow tract is also enlarged to enhance blood flow, is performed in infancy, the pulmonary autograft may grow proportionally with somatic growth.
4. Autograft stabilization in adolescents appears as important as it is in adults, especially for patients with significant preoperative aortic insufficiency.
5. Primary aortic valve repair or percutaneous aortic balloon valvuloplasty does not prevent the Ross operation from being done, and results with the Ross operation after these procedures are excellent in experienced units.
6. In institutions with significant expertise, mortality after both aortic valve repair and Ross operation is mainly driven by concomitant anomalies.
7. Mortality after both aortic valve repair and Ross operation remains high in neonates and infants when performed outside the institutions with significant expertise.
In recent years, when aortic valve repair has been performed in neonates and infants with isolated aortic stenosis, later aortic valve replacement isn’t always necessary. One study found that when optimal repair was achieved in these patients, 80% were free from reoperation at 10 years.
Advertisement
On the flip side, some emerging data suggest that a Ross performed in infancy may allow normal growth of the neoaortic root without need of subsequent stabilization.
Dr. Najm notes that many factors play into the decision, including heart function, the child’s functional status, and other associated conditions. “We put a lot of thinking into what is the best procedure for a given patient. It’s a balance.”
While the writing panel members were not always in agreement, Dr. Najm says there was one solid area of consensus: “If the valve is not amenable to repair in a growing child, the Ross procedure is definitely the right operation. There’s nothing better.”
Advertisement
Advertisement
Join us in New York City Dec. 5-6
Choice between smaller or larger prosthesis is a tradeoff between leak and pacemaker risks
4-D imaging informs complex aortic valve repair in adult and pediatric patients
Study offers guidance on an increasingly common presentation
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
Series of 145 patients characterizes scope of presentations, interventions and outcomes
Experience-based takes on valve-sparing root replacement from two expert surgeons