Research shows procedure is safe and effective

Cleveland Clinic doctors have published the first study illustrating the safety and efficacy of endoscopic needle knife therapy for intestinal strictures in patients with inflammatory bowel disorder (IBD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We pioneered this procedure,” says Bo Shen, MD, Medical Director of Cleveland Clinic’s IBD Center. “And our research shows that it is effective and can have advantages over other conventionally used treatments, such as medical therapy, balloon dilation and surgery.”
Shen’s study, which was co-authored with research fellow Nan Lan, MD, was featured as the cover story in the April 2017 issue of the journal Inflammatory Bowel Diseases. Dr. Lan will present their findings in May at DDW 2017.
In their study, Drs. Shen and Lan reviewed the records of 85 patients with strictures treated by needle knife stricturotomy (NKSt) between 2008 and 2016 at Cleveland Clinic’s Center for Inflammatory
Bowel Disease.
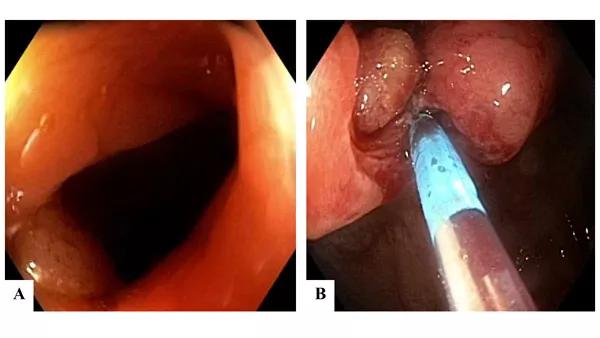
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b39bacf6-ca7b-4539-bdda-23c1141a8868/17-DDI-346-Shen-CQD-Inset_jpg)
Because many patients had multiple strictures, there were a total of 231 NKSts performed on the 85 subjects. Passage of the scope through each stricture was achieved in 100 percent of the patients. Delayed bleeding occurred in nine cases and perforation occurred in one, requiring hospitalization.
Developing nonsurgical treatments for IBD patients such as NKSt results in better quality of life, Dr. Shen says. “Multiple bowel resection surgeries can shorten patients’ intestinal tracts while noninvasive procedures preserve them.”
Strictures, the narrowing of the intestines due to inflammation and scarring, are a common side effect of IBD. Patients with Crohn’s disease or, to a lesser degree, ulcerative colitis after surgery, often develop them as their conditions progress. Strictures also may occur after a bowel resection. They can cause abdominal pain, diarrhea, nausea, vomiting, weight loss and malnutrition.
Advertisement
To treat strictures, physicians typically have turned to surgery or a procedure called endoscopic balloon dilation (EBD) that stretches out the constricted area, however, this therapy carries a risk of perforation and intestinal bleeding, and usually the therapeutic effect typically lasts only three to six months before the stricture returns.
The interval between endoscopic and surgical interventions and the interval from the treatment to the return of the stricture was longer, Drs. Shen and Lan found, if patients first had NKSt. “For example, if you need EBD every three months, you need it every six months after NKSt,” Dr. Shen says.
Dr. Shen was already experienced in using endoscopic needle-knife technology to treat strictures in the upper GI tract when he decided it might be a good alternative therapy for IBD patients with strictures in the lower GI track.
He says the technology allows physicians to be much more precise when opening up strictures. “You have more control over how deep you cut and where you cut,” he says, pointing out that if a patient has a stricture close to the anus, there is a risk of rectovaginal fistula from blind balloon dilation therapy, which can result in bowel movements leaking into the vagina.
“With the needle knife, you can avoid the front wall of the rectum,” Dr. Shen says. “You cut only the back wall, so you can avoid these complications. This is a major advantage.”
Physicians from around the world have come to Cleveland Clinic to learn NKSt.
“It’s a procedure with some risks involved,” Dr. Shen says. “So intense training is important.”
Advertisement
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications