Study helps identify patients likely to benefit from continuous monitoring

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/658fec96-ec9a-4849-b332-3b354754f2da/17-PAI-1319-Khanna-Hero-Image-650x450pxl_jpg)
17-PAI-1319-Khanna-Hero-Image-650x450pxl
A patient is recovering from surgery in a hospital’s general care unit (surgical floor/ward). At regularly scheduled intervals, a nurse (or nonlicensed healthcare provider) enters the patient’s room to check blood pressure, heart rate, respiratory rate and oxygen saturation. The nurse may also ask about pain, mental status and other prespecified parameters in specific cases. While everything may seem fine at these snapshots in time, there may be intervals in between these checks where the patient’s oxygen saturation is intermittently dropping and/or the patient is not taking adequate tidal volume breaths.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The problem? No one will notice until the next regularly scheduled room visit. Or until the patient starts to develop a serious cardiorespiratory crisis or near flatline status. At this point, it may be too late…
Serious issues can arise when oxygen saturation drops in combination with a shallow and less-than-adequate respiratory drive, which leads to hypercapnia. Repetitive and prolonged episodes of dangerous deviations from the norm may also compromise cardiac function, leading to cardiorespiratory decompensation. Once excessive demand has been placed on the patient’s cardiorespiratory function, patients often go into cardiac arrest. Recent literature spread over the last decade has identified that acute respiratory events on inpatient wards in the U.S. are common, with an associated in-hospital mortality of approximately 40 percent. Even without mortality, these critical patients end up as unprecedented admissions in the ICU, draining manpower and other resources in the ICU — a place that should be reserved for true emergencies.
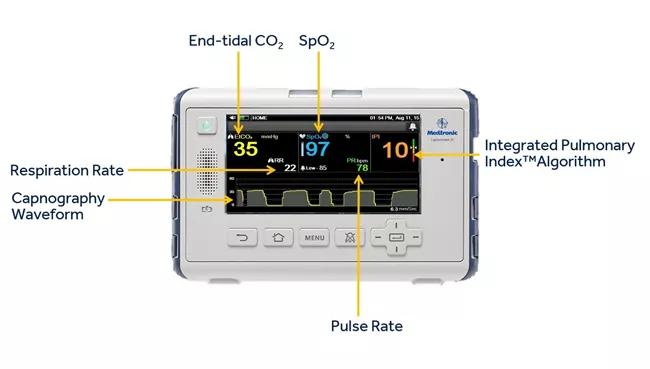
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/10dc457c-d0c7-4221-ad6e-c1c79e5c57b4/17-PAI-1319-Khanna-Inset-Image-650pxl-width-002_jpg)
“While general care units are designed for patients who are basically stable, it doesn’t mean we should compromise on their monitoring — especially if there’s enough lead time to indicate when things are going wrong,” explains Ashish Khanna, MD, FCCP, FCCM, Staff Intensivist and Vice-Chief for Research at Cleveland Clinic’s SICU & Center for Critical Care. “If there’s any chance that a patient could decompensate suddenly, we need to take advantage of technology that allows us to monitor and prevent critical incidents from occurring. And we need to do this proactively if we truly want to make a difference in outcomes.” (Figure above is CAPNOSTREAMTM 35 portable respiratory monitor from Medtronic.)
Advertisement
To combat these issues, researchers have identified some potential benefits of continuous monitoring. However, potential issues involve identifying who to monitor as well as what and how to monitor, given the major infrastructure support this kind of change would entail. To justify significant changes nationwide, researchers are looking for ways to predict the likelihood of cardiorespiratory events and optimize the monitoring process. The ultimate goal is to develop a smart, continuous monitoring platform that allows for safer patient recovery without burdening healthcare providers in the general care units with false alarms and alarm fatigue.
Under the leadership of Principle Investigator Dr. Khanna, Cleveland Clinic recently contributed to an international trial designed to generate a risk prediction score based on continuous monitoring data. The Prediction of Opioid-induced Respiratory Depression In Patients Monitored by capnography (PRODIGY) trial is the first study of continuous (yet blinded) multiparameter cardiorespiratory monitoring of this size ever conducted. The trial involved nearly 1,500 patients across 16 different sites and three continents. About a fifth (nearly 300) of these patients were from Cleveland Clinic. Dr. Khanna was also a part of a three-member trial steering committee and was instrumental in the design and construct of the trial idea and overall concept of PRODIGY.
The study involved continuous, blinded cardiorespiratory monitoring of all patients (including surgical and medical) receiving opioid-based pain medication on the regular hospital floor. The monitor screens were covered and the alarm capacity was silenced so that the true pattern of events and the burden of the problem could be uncovered at the time of final analysis. Continuously monitored data was collected for oxygen saturation, respiratory rate, heart rate and end-tidal carbon dioxide levels along with integrated pulmonary index (a derived parameter from these values). However, standard-of-care monitoring continued in the usual unblinded fashion throughout, and patient safety was never compromised in any way.
Advertisement
Through pattern detection analysis, the collected data was used to develop a unique prediction model and a novel risk prediction score (PRODIGY score). This model and score help identify the patients who are most likely to decompensate and thereby may benefit the most from continuous monitoring. Full trial results are expected to be published by the end of 2018.
“While there are other scores used to predict respiratory compromise after surgery, our study was the first to provide a risk prediction model based on scores obtained from real-time monitoring data that uncovered several concerning patterns not seen before,” notes Dr. Khanna. “Since it’s very expensive to put every patient on continuous monitoring, we can use our score and prediction model to identify the patients who are most likely to decompensate. The study is also unique in looking at a cohort of medical inpatients on opioids as well and identifying a model to predict cardiorespiratory compromise in these patients. This has not been done prior to PRODIGY.”
In the future, additional research and education efforts will be made to support the widespread adoption of continuous monitoring. Consider the following examples:
Advertisement
Advertisement
Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies
Study participants also reported better sleep quality and reduced use of pain medications
Two-hour training helps patients expand skills that return a sense of control
Program enhances cooperation between traditional and non-pharmacologic care
National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS
Pain specialists can play a role in identifying surgical candidates
Individual needs should be matched to technological features
New technologies and tools offer hope for fuller understanding