Urologic surgeon at Cleveland Clinic Indian River Hospital performs irreversible electroporation for select cases of localized prostate cancer.
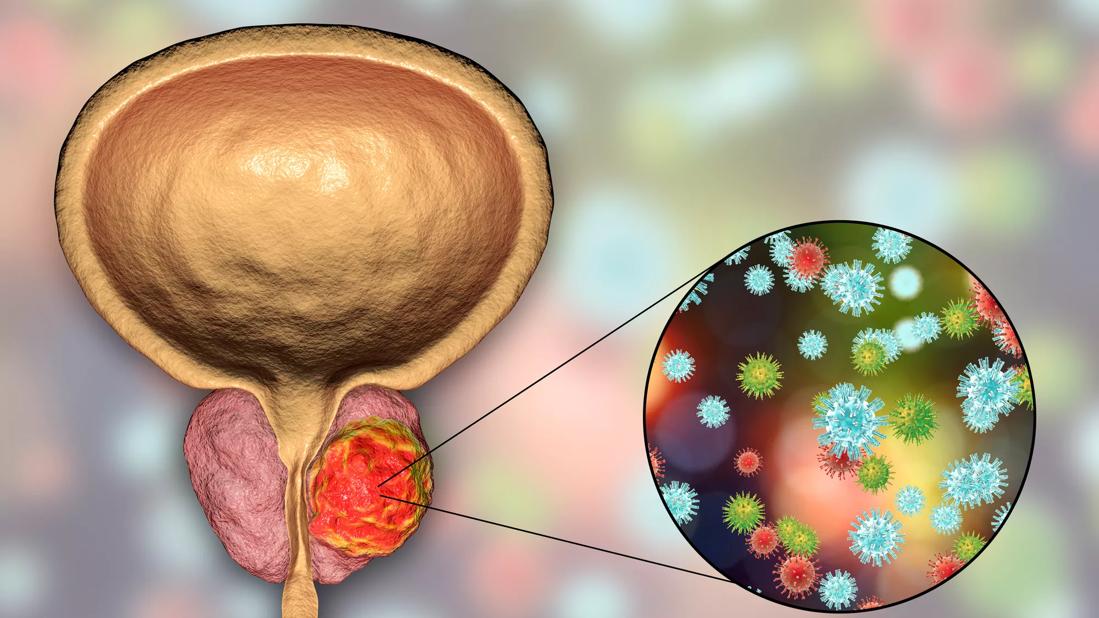
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/76eef579-9f20-4b97-aa6f-e277461a6efb/GettyImages-872569336-jpg)
Prostate Cancer
The last decade has seen a marked shift in the treatment of prostate cancer. Fewer people are undergoing routine screening and more are choosing active surveillance over surgery or radiation. When radical prostatectomies are performed the vast majority are robotic assisted. And now there is a growing category of focal therapies emerging as alternatives to whole-gland therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One of those focal therapies, irreversible electroporation (IRE), is performed at Cleveland Clinic Indian River Hospital by board-certified urologic surgeon Jamil Syed, MD. IRE is a novel non-thermal ablative technique that uses pulses of electric current to target cancerous tissue in the prostate while preserving the rest of the gland.
Fewer than 200 surgeons across the country perform IRE using the NanoKnife® System, and Dr. Syed is the only Cleveland Clinic surgeon in Florida currently offering this treatment option. He trained in the procedure during his urology residency and general surgery internship at Yale New Haven Hospital, prior to joining Cleveland Clinic in 2022.
“Focal therapy is a good option for a highly select group of patients with localized low- and intermediate-risk prostate cancer,” states Dr. Syed. “These are often individuals who are not comfortable with monitoring alone but do not want to face the potential side effects of more aggressive treatments.”
IRE is a surgical approach that involves going through the perineum to place 2 to 6 monopolar probes within a target area of tissue based on multiparametric magnetic resonance imaging (mpMRI) and ultrasound-guided biopsy. Dr. Syed then delivers a series of high-voltage direct current pulses between the electrodes. This creates nanopores in the membrane of the cancer cells leading to permanent cell death.
“IRE allows me to ablate the cancer while preserving nearby connective tissue and minimizing nerve damage,” explains Dr. Syed. “This form of focal therapy lessens the risk of complications, such as urinary incontinence and erectile dysfunction, seen with traditional treatments and also allows for a quicker recovery.”
Advertisement
He describes patients experiencing just a couple nights of soreness after the outpatient procedure, which is performed under general anesthesia.
According to Dr. Syed, the use of IRE in the management of localized prostate cancer should be based on risk factors and patient characteristics. Candidates should have unilateral cancer or cancer in just one quadrant of the prostate with biopsy-confirmed lesions visible on MRI scans.
“I offer this approach for certain patients with localized intermediate-risk prostate cancer, and only in very rare cases would I offer it to a patient with low-risk disease,” says Dr. Syed.
He points to improved diagnostic tools and risk stratification methods, such as advanced genomic testing and better biopsy techniques, that allow identification of patients who may benefit most from focal therapy versus standard treatments.
Close to 300,000 new cases of prostate cancer will be diagnosed in the United States in 2024, reports the American Cancer Society. Of those, less than 30% will have low-risk disease, according to an analysis of the Surveillance, Epidemiology, and End Results (SEER) database that looked at prostate cancer diagnoses from 2004 to 2014. About half will have intermediate-risk disease and the remainder high risk.
Current AUA/ASTRO guidelines, updated in 2022, recommend active surveillance for patients with low-risk prostate cancer, which involves closely monitoring the cancer (serial PSA values and repeat prostate biopsy) without immediate treatment. The guidelines strongly recommend “patients with unfavorable intermediate- or high-risk prostate cancer and estimated life expectancy greater than 10 years,” receive a choice between radical prostatectomy or radiation therapy plus androgen deprivation therapy (ADT).
Advertisement
For patients with favorable intermediate-risk prostate cancer, at lower risk of the cancer spreading beyond the prostate, the guidelines recommend a discussion of active surveillance, radiation therapy, and radical prostatectomy. They only endorse the use of focal therapy in a research or clinical trial setting.
“Some of the most in-depth conversations I have are with individuals with intermediate-risk disease because their road forward is less clear,” notes Dr. Syed. “I appreciate being able to offer some of them a middle ground with focal therapy.”
During these discussions, Dr. Syed makes it clear that IRE is considered investigational and not yet part of standard therapy. The NanoKnife System is FDA-approved for the surgical ablation of soft tissue, but has not yet received clearance for the treatment of any specific disease or condition.
“Focal therapies, like IRE, are considered less effective than whole-gland therapies, so it’s important for patients to weigh the potential benefits and risks,” says Dr. Syed.
He also emphasizes to patients that they must be closely monitored after focal therapy to evaluate the oncological effectiveness of treatment, look for signs of cancer recurrence, and to identify any new cancer that may develop in untreated areas of the prostate.
“If the cancer does return, patients are still eligible for salvage therapy with radical prostatectomy or radiotherapy,” adds Dr. Syed.
He also points out that about a third of patients who choose active surveillance will have definitive treatment within 10 years. “So many of these conversations happen across multiple visits over multiple years,” he says.
Advertisement
While there is currently a lack of high-quality data comparing focal ablation outcomes to radiation therapy, surgery, and active surveillance, the short-term oncologic effectiveness of IRE has been demonstrated via multiple studies.
For example, an Australian study published in 2023 looked at the median 5-year outcomes of IRE for patients with localized prostate cancer. The study included 229 patients, most of whom (86%) had intermediate-risk prostate cancer. The failure-free survival was 91% at 3 years, 84% at 5 years and 69% at 8 years. The metastasis-free survival was 99.6% and the prostate cancer specific and overall survival were 100%. The researchers also found erectile function was preserved in 87% of men and continence was close to 100%.
In addition, preliminary results of PRESERVE, the first, large, United States-based trial evaluating IRE in patients with intermediate-risk prostate cancer, were published earlier this year. They demonstrated that IRE can be performed safely, but oncological and quality of life outcomes at 12 months are currently pending. The researchers noted, however, initial decreasing PSAs are an early indication of ablation treatment efficacy.
A team of physician-researchers at Cleveland Clinic in Ohio also is collecting data on patients treated with IRE to determine long-term safety and efficacy of this novel focal ablative technique.
Advertisement
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.