Surgeons at Cleveland Clinic Weston Hospital demonstrate the latest approaches to treating gynecological cancer
Surgeons at Cleveland Clinic Weston Hospital combined robotic-assisted cytoreductive surgery with laparoscopic hyperthermic intraperitoneal chemotherapy (HIPEC) for the first time to treat a patient with advanced ovarian cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Board-certified gynecologic oncologist Joel Cardenas Goicoechea, MD, MBA, collaborated with Conrad H. Simpfendorfer, MD, FACS, Director of Hepatobiliary & Pancreas Surgery, on the novel case, demonstrating the latest approaches to treating the most lethal gynecologic cancer.
Ovarian cancer was responsible last year for more than 13,000 deaths and nearly 20,000 new diagnoses in the United States, according to American Cancer Society estimates. While ovarian cancer diagnoses and deaths have been declining for the past two decades, the overall five-year survival of epithelial ovarian cancer (EOC) -- the most common type -- remains around 50%.
“For metastasized disease, the five-year survival rate drops to about 30%,” notes Dr. Cardenas. “Unfortunately, about 75% of patients have stage III or stage IV disease at diagnosis, which comes with a high reoccurrence rate.”
Laparotomy is the current standard of care for advanced stage ovarian cancer. While these cases are traditionally treated with surgery up front, some patients benefit from platinum-based chemotherapy and open interval debulking surgery (IDS). But a number of small studies have demonstrated that minimally invasive interval cytoreduction may be able to achieve a high rate of complete cytoreduction along with better perioperative outcomes.
“Right now most patients with ovarian cancer have open surgery to achieve maximal debulking, but in very select cases we can use a minimally invasive approach,” says Dr. Cardenas. “Appropriate cases for a robotic approach require a positive response to neoadjuvant chemotherapy, no ascites, a tumor size under 10 cm, normalization of CA 125, and tolerance of the Trendelenburg position.”
Advertisement
Dr. Cardenas has performed about two dozen robotic-assisted surgeries for ovarian cancer in addition to many laparoscopic procedures. “The advantages of a robotic approach over laparoscopy include 3D visualization and improved depth perception as well as increased dexterity,” he says.
In a retrospective study of his first 12 cases using robotic-assisted interval cytoreductive surgery, prior to joining Cleveland Clinic, Dr. Cardenas achieved optimal cytoreduction in 100% of patients and complete cytoreductive in 75% of patients.
More recently, researchers completed the feasibility phase of the Laparoscopic Cytoreduction After Neoadjuvant Chemotherapy (LANCE) trial, an international, prospective, randomized, multicenter, non-inferiority phase III trial to compare MIS versus laparotomy in women with advanced stage high-grade EOC. Having achieved complete gross resection in 87.5% of patients assigned to MIS surgery (laparoscopic or robotic) versus 83% in the open group (p=0.6), researchers are proceeding with the definitive trial to determine if MIS after chemotherapy can prolong the return of the disease and/or improve quality of life after surgery.
In other efforts to lengthen recurrence-free survival, the National Comprehensive Cancer Network’s 2019 guidelines were updated to include HIPEC following IDS as a therapeutic option for women with stage III ovarian cancer who have a response or stable disease after 3 to 6 cycles of neoadjuvant chemotherapy (NACT).
The guidelines cited positive findings from multiple prospective studies, including the landmark multicenter, randomized phase III trial by Van Driel et al. published in 2018, which found HIPEC resulted in longer recurrence-free survival and overall survival without higher rates of side effects.
Advertisement
“The goal of HIPEC is to target residual disease following cytoreductive surgery by perfusing the peritoneal space with a heated solution of chemotherapy agent for 60 to 90 minutes,” explains Dr. Simpfendorfer, an early adopter who helped launch Cleveland Clinic’s HIPEC program in Florida in 2015.
Research has shown that peritoneal metastases are difficult to treat systemically due to poor blood supply to the peritoneal surface and low drug penetration. “That same absorption barrier benefits patients by reducing HIPEC side effects and toxicity,” says Dr. Simpfendorfer.
Originally established to treat GI malignancies confined to the peritoneal cavity, including colon, gastric and appendiceal cancers, the HIPEC program at Weston Hospital was expanded last year to include select cases of advanced and recurrent ovarian cancer.
“About 70% of our HIPEC cases are for the treatment of colorectal cancer that has spread to the abdominal cavity and very few cases are performed laparoscopically,” notes Dr. Simpfendorfer.
In October 2023, Dr. Cardenas teamed with Dr. Simpfendorfer on a unique case in which they combined robotic-assisted cytoreduction surgery with laparoscopic HIPEC. Referred by a colleague at Cleveland Clinic Indian River Hospital, the 81-year-old patient was diagnosed with stage III EOC. Because she was not a candidate for primary debulking surgery, the patient first underwent NACT with paclitaxel and carboplatin.
“The patient had a remarkable response following 6 cycles,” describes Dr. Cardenas. “There was a decrease in her tumor burden, her ascites resolved, and she experienced symptom reduction in terms of girth and pain. Plus her CA 125 blood test returned to a normal range.”
Advertisement
Subsequently, the patient was determined to be an ideal candidate for both a robotic-assisted surgical approach and laparoscopic HIPEC. “Prior to this case, our team had performed about 10 cases of open debulking surgery for ovarian cancer followed by open HIPEC. This was our first fully ‘closed’ case,” remarks Dr. Cardenas.
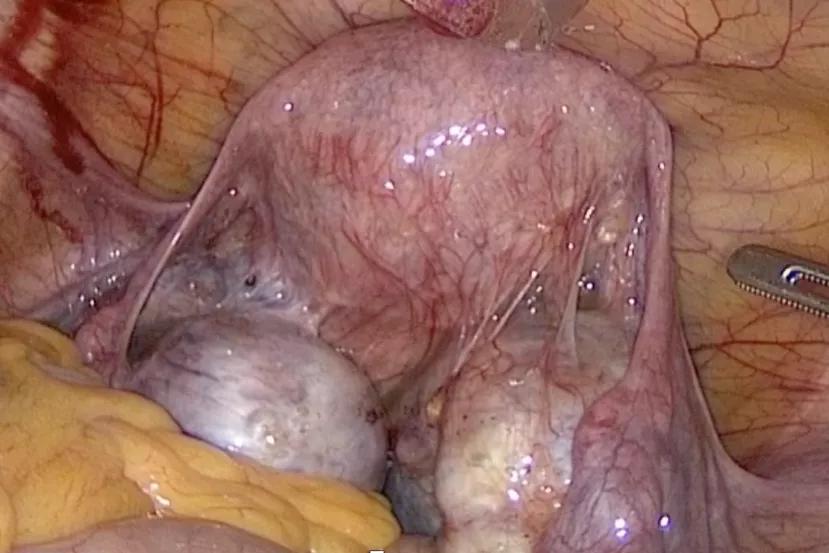
Using the da Vinci Xi surgical system, Dr. Cardenas performed a total hysterectomy and bilateral salpingo-oophorectomy, followed by an omentectomy and removal of the diseased portions of the peritoneum.
“We were able to easily rotate the boom and redock as we transitioned between the pelvic approach to the abdominal portion of the surgery,” explains Dr. Cardenas. “Though it was a highly complex surgery, the robotic surgical system provided excellent access, and I was able to resect 100% of the tumor.”
The surgical component of treatment lasted approximately 4 hours and was immediately followed by a 90-minute course of HIPEC with cisplatin (100 mg/m2) heated to 42°C. “We used two of the existing 8 mm access points to position the two catheters for introduction and removal of the chemotherapy agent,” says Dr. Simpfendorfer.
To reduce HIPEC-related complications, the patient’s urine output was continuously monitored during the procedure and her core body temperature was closely controlled with the application of ice packs to the neck and groin regions. Steroids were also given after the surgery to combat nausea and vomiting side effects.
According to Dr. Cardenas, the patient had no surgical complications, and she remained in the hospital for just 3 days. Typically, patients who undergo laparotomy have an average hospital stay of 8 to 10 days, and even longer with the addition of HIPEC.
Advertisement
“With robotic-assisted surgery, patients usually experience reduced blood loss, fewer complications, less postoperative pain, and a faster recovery,” says Dr. Cardenas. “Some also have a shorter downtime before resuming chemotherapy.”
He credits the patient’s rapid recovery, in part, to having an excellent performance status prior to treatment. “She is doing very well today under the care of a medical oncologist as she completes 3 additional cycles of chemotherapy,” he says, noting the patient will also receive treatment with PARP inhibitors for up to three years.
Time will tell if the unique treatment combination extends the patient’s progression free survival, but Dr. Cardenas is optimistic.
For more information, visit Cleveland Clinic Florida ConsultQD. Subscribe to the Florida Physician Newsletter.
Additionally, follow us on X (formerly Twitter), Facebook, and LinkedIn.
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.