Editorial lays out best practices from three Cleveland Clinic surgeons
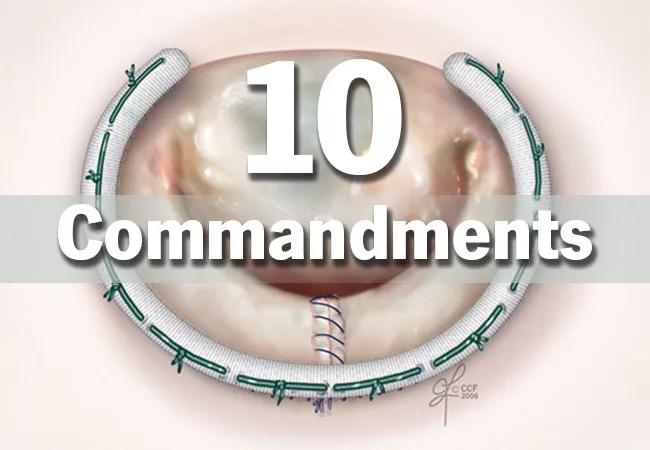
With a variety of options available to address a prolapsed mitral valve, repair is feasible in more than 95% of cases and yields better outcomes than replacement. In a new editorial, “The 10 Commandments for Mitral Valve Repair,” published in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery, three Cleveland Clinic cardiothoracic surgeons detail critical recommendations for successful repair.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Mitral regurgitation from degenerative disease can be repaired equally well via a variety of different surgical techniques,” says lead author A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “But whichever technique is chosen, the surgeon must follow certain guidelines to ensure a safe and successful repair.”
The editorial’s 10 commandments are briefly recapped below
Together, the surgeon and echocardiographer should evaluate the baseline transesophageal echocardiogram for the following:
Complete interrogation of the mechanism of regurgitation is most important, with evaluation including two- or three-dimensional echocardiography with and without color flow.
The choice between a full sternotomy or a less-invasive option depends on patient anatomy and physiology as well as the surgeon’s skill and comfort level. “Safety is the first priority,” says editorial co-author Daniel Burns, MD, MPhil. “It is crucial to remember that as the approach becomes less invasive, control over the operation is necessarily relinquished. Early in a surgeon’s experience, it is unwise to tackle a complex valve repair with a minimally invasive approach for the sake of pushing the envelope, as this can prolong cross-clamp time and may risk limb ischemia and other adverse events.”
The authors recommend a sternal approach for patients with aortic insufficiency greater than 1+, severe mitral annular calcification, left ventricular dysfunction or dilatation, pulmonary hypertension, aorto-iliac atherosclerosis or femoral artery diameter less than 7 mm.
Advertisement
While robotic surgery nearly always provides excellent exposure, patients with obesity or a severe pectus excavatum should undergo standard sternotomy. In general, a left atriotomy provides the best valve exposure. However, for challenging cases (e.g., a small left atrium), a trans-septal approach may be a justified trade-off for optimal visualization despite the increased risk for postoperative dysrhythmia and need for a permanent pacemaker.
For nonrobotic approaches, placing the annuloplasty sutures first — with the first one placed wherever is easiest — enhances exposure for a more complete valve inspection. Directing needle tips toward the valve/ventricle when placing sutures in the annulus near the orifice of the left atrial appendage and left fibrous trigone avoids damaging the circumflex coronary artery.
With the echocardiogram findings in mind and valve exposure optimized, inspection should include detecting leaks (using a saline test), identifying areas of prolapse and ruptured chordae, and noting indentations, clefts and areas of leaflet restriction. A tall posterior leaflet is associated with SAM and requires preventive measures.
“For isolated posterior leaflet prolapse, either resection or creation of artificial chords will lead to good outcomes, so surgeons should choose techniques they are comfortable with,” urges editorial co-author Per Wierup, MD, PhD. For anterior leaflet prolapse, however, he recommends artificial chordae creation.
Assessing chordal length is cited as the biggest challenge in creating artificial chordae. The loop technique enables premeasurement to the length of the native chordae; if chordae are constructed freehand, the final length should be adjusted after the annuloplasty has been secured.
Advertisement
A prosthetic annuloplasty should be inserted for all repairs for degenerative disease, but the choice of ring versus band and rigid versus flexible are a matter of preference. The authors favor a flexible band for most cases. While sizing should be determined based on the surface area of the anterior leaflet, a relatively large band or ring is appropriate for most patients.
“Although there is no way to completely avoid the risk of SAM in mitral valve surgery, efforts should be made to minimize it,” says Dr. Gillinov. This begins with evaluating the preoperative echocardiogram for the following:
If any two of these features are present, preemptive surgical measures are needed to move the point of coaptation posteriorly by avoiding too small of an annuloplasty and reducing posterior leaflet height.
Full ventricular recovery must take place before final weaning from cardiopulmonary bypass. This requires time, a high systemic blood pressure and, in some cases, inotrope administration.
Anything higher than mild (1+) mitral regurgitation following repair is almost always unacceptable, the authors assert. And even that level should prompt careful study of the echocardiogram and a possible second pump run to identify problems for immediate correction.
“Good long-term outcomes start with good short-term results,” concludes Dr. Gillinov. “These preoperative and intraoperative ‘commandments’ optimize success for our patients.”
Read the full editorial here.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more