A review of the latest data

By Demetrius Coombs, MD, Ritwik Grover, MD, and Raffi Gurunluoglu, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Women receive breast implants for both aesthetic and reconstructive reasons. This brief article discusses complications related to breast implants.
Capsular contracture is the most common complication of breast augmentation. Other complications include infection, malposition, rippling, seroma, hematoma and sensory alterations.
Irrigation during the implantation procedure with a triple antibiotic solution consisting of bacitracin, gentamycin and cephalexin in normal saline decreases infection and seroma rates.
Some surgeons also choose to irrigate the pocket with a betadine solution, or to cleanse the skin with betadine and place sterile towels and redrape before inserting the implant. Additionally, many prefer using a sterile device much like a pastry funnel called a Keller funnel to insert the implant into the breast pocket.
Infection is less common with cosmetic augmentations than with implant-based breast reconstruction, likely because of healthier, well-vascularized tissue in patients undergoing cosmetic surgery than in those undergoing mastectomy.
Seroma is thought to be a consequence of texturing, and more so with macro- vs microtexturing. Though poorly understood, an association between texturing and double capsules has also been reported.
After primary breast augmentation, 10-year follow-up rates of capsular contracture, seroma, rippling and malposition vary across the three major silicone implant manufacturers. Hematoma and infection occur in less than 1% of primary augmentation patients.
Advertisement
Malposition of the implant over time is less frequent with textured implants because of the higher coefficient of friction compared with smooth implants.
Visible skin rippling may be a consequence of texturing and also of thin body habitus, e.g., in patients with a body mass index less than 18.5 kg/m2. If the soft-tissue layer of the breast is thin, the natural rippling of smooth saline implant shells are more likely to show when placed in the subglandular pocket. Form-stable implants, by contrast, resist rippling.
Large implants and extensive lateral dissection can cause alterations in nipple sensation and sensory loss within lower breast pole skin. Axillary incisions may traumatize or damage the intercostobrachial nerve, resulting in upper inner arm sensory aberrations.
Ultimately, the 10-year incidence of secondary surgery ranges from 0% to 36% and the 10-year incidence of capsular contracture ranges from 11% to 19%. Additional cosmetic complaints after augmentation with implants include enlargement of the areola and engorgement of breast veins.
Although concerns persist, multiple studies have demonstrated the safety of fourth- and fifth-generation silicone breast implants with regard to autoimmune disease.
In various clinical studies in mastectomy patients who underwent breast reconstruction with either silicone implants or autologous tissue, no difference was found with regard to the incidence of autoimmune diseases. Additionally, in meta-analyses of data from more than 87,000 women, no association was found between connective tissue disease and silicone breast implants. One study noted no increase in autoantibodies in patients with undamaged silicone implants vs patients who experienced rupture.
Advertisement
Studies have also demonstrated that in children born to mothers with breast implants, the risk of rheumatic disease, esophageal disorders, congenital malformations and death during the perinatal period is comparable with that in controls. Another study, examining breastfeeding in women with silicone breast implants, showed no significant difference in silicon levels (used as a proxy for silicone) in breast milk compared with controls without implants; silicon levels were found to be significantly higher in cow’s milk and store-bought formulas.
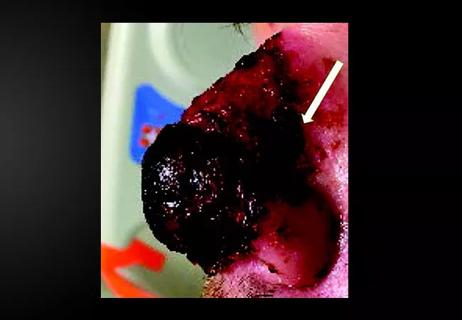
Breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) is a subtype of T-cell lymphoma that develops in tissue adjacent to breast implants. It typically presents as breast swelling two to 38 years (mean of eight years) after implant insertion. The swelling may be secondary to periprosthetic seroma formation or, more rarely, palpable disease in the axilla. Patients occasionally complain of pain and, rarely, constitutional symptoms. BIA-ALCL is not a disease of the surrounding breast tissue, but rather of the fibrous periprosthetic capsule.
Of note, there is no documented case involving smooth implants, but it may be related to fifth-generation textured implants. At present, it is not possible to definitively state which implant is associated with this condition; hence, more data are needed, and this association is currently under study.
The absolute risk of BIA-ALCL was reported in a Dutch study as 1 in 35,000 by age 50, 1 in 12,000 by age 70, and 1 in 7,000 by age 75, with a number needed to harm of 6,920. Overall lifetime risk was estimated at 1 in 30,000 for women with textured implants in a 2015 U.S. study. In comparison, breast cancer risk is about 1 in 8 women. There is no apparent predilection for patients who underwent cosmetic augmentation versus reconstruction, or who received silicone versus saline implants.
Advertisement
The mechanism of this malignancy is currently under investigation, but the current theory implicates an exaggerated lymphoproliferative response to bacterial contamination of the capsule superimposed upon genetic factors in susceptible patients.
National societies advise plastic surgeons to discuss the risk of BIA-ALCL with all patients at the time of breast augmentation consultation and to report all confirmed cases to the PROFILE registry (Patient Registry and Outcomes for Breast Implants and Anaplastic Large Cell Lymphoma Etiology and Epidemiology).
Drs. Coombs and Ritwick are plastic surgery residents. Dr. Gurunluoglu is staff in the Department of Plastic Surgery.
This abridged article was originally published in Cleveland Clinic Journal of Medicine.
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair