Cortical-sparing surgery may be best option
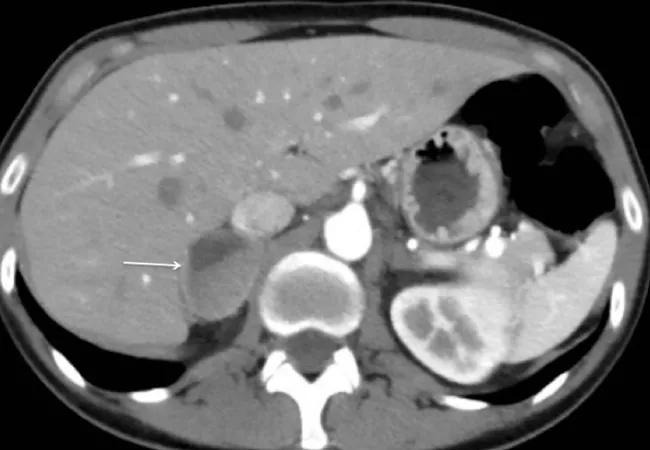
While many tumors of the adrenal gland are noncancerous, they can cause life-threatening disease due to an overproduction of “fight-or-flight” hormones. One such tumor type is called pheochromocytoma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pheochromocytomas are complex catecholamine-secreting tumors of the adrenal medulla with an annual incidence of two to eight cases per million. They affect the medulla and cause an overproduction of adrenaline, which can lead to hypertension, profuse sweating, headaches, panic attacks, arrhythmia, stroke and even death. Many of the tumors are sporadic in nature, while at least half are associated with a genetic disorder. Patients with disease-causing gene mutations are at higher risk for developing subsequent tumors.
The current standard treatment for pheochromocytoma affecting both adrenals is bilateral adrenalectomy. While this treatment eliminates the potential of developing new tumors, patients require life-long hormone replacement therapy to compensate for the loss of their adrenal function.
Recent data suggest that preserving as much of the adrenal cortex as possible (cortical-sparing adrenalectomy) can reduce the need for hormone replacement therapy, which in itself presents unique health risks. However, evidence for clinically recommending this procedure is weak, as the risk of tumor recurrence and metastasis is higher and long-term efficacy is not well understood.
To address this knowledge gap, an international team of researchers co-led by Charis Eng, MD, PhD, Chair of Cleveland Clinic’s Genomic Medicine Institute, analyzed long-term outcomes in 625 patients with bilateral pheochromocytomas who underwent total or cortical-sparing adrenalectomy. Published in JAMA Network Open, the results show that hormone therapy after bilateral total adrenalectomy resulted in adrenal crisis or Cushing syndrome. Conversely, the cortical-sparing procedure was not associated with worse outcomes or higher morbidity, even when tumors recurred.
Advertisement
Furthermore, cortical-sparing adrenalectomy may be ideal for individuals with hereditary pheochromocytoma as they are at higher risk for developing new tumors that would require additional surgeries. Genetic analyses of the study participants revealed a high percentage (96%) of patients had germline mutations associated with bilateral pheochromocytoma; however, clinical features of predisposing mutations are not always evident.
“For example, many patients who eventually develop bilateral pheochromocytoma often present for the first time with only one pheochromocytoma affecting one adrenal gland. When this occurs, surgeons often perform total adrenalectomy,” explains Dr. Eng. “This is problematic when the second pheochromocytoma occurs in the opposite gland, leaving few options. Therefore, we recommend that all patients presenting with pheochromocytomas should be offered genetic analysis to guide surgical and medical management decisions. This is because genetic disease increases the risk of bilateral pheochromocytoma.”
In summary, the multidisciplinary group of researchers concluded that cortical-sparing surgery can be appropriate and safe for certain cases of bilateral pheochromocytoma, particularly when a predisposing mutation is present. Since clinical features of predisposing mutations are not always evident, this study underscores the importance of genetic testing in diagnosing and managing pheochromocytoma.
“At Cleveland Clinic, all patients with pheochromocytoma are referred to genetics,” states Eren Berber, MD, a surgeon in Cleveland Clinic’s Department of Endocrine Surgery. With five specialized endocrine surgeons committed to best practices and superior outcomes, the group is one of the busiest in the world and at the forefront of emerging treatments, technology and surgical approaches, including robotic surgery. According to Dr. Berber, the department performs approximately 80 adrenalectomies per year, and they follow the recommendations of this study.
Advertisement
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications