Cleveland Clinic endocrinologists work to identify protocols for improving care
For patients with diabetes, hospital stays can disrupt stable blood glucose control. Regardless of what prompts hospitalization, new procedures and medications — along with transitions between departments and eventual discharge — create the potential for hyperglycemic events that can result in prolonged stays or readmissions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With a focus on research, technology and team-based care, researchers at Cleveland Clinic’s Endocrinology & Metabolism Institute are investing in efforts to improve glucose management during hospital transitions.
Across healthcare, providing better in-hospital glucose management must begin with more robust data, says Keren Zhou, MD, Research Director.
“Hyperglycemia in hospitals is an important issue,” says Dr. Zhou. “In terms of frequency, we are seeing alarming trends in very high levels of hyperglycemia in the hospital that are not necessarily improving over time.”
Among patients with diabetic ketoacidosis and type 1 diabetes, 20% are readmitted within 30 days of discharge, and more than 80% will have one to three admissions in the year after their sentinel admission, says Dr. Zhou.
“Very little has been published on what processes can reduce readmission, so we aim to see whether the utilization of multidisciplinary teams of physicians, diabetes educators and pharmacists, along with use of continuous glucose monitoring, can assist in reducing these readmission rates,” she says.
Hyperglycemia in the hospital is associated with increased morbidity such as higher rates of infection and cardiac events, says Dr. Zhou.
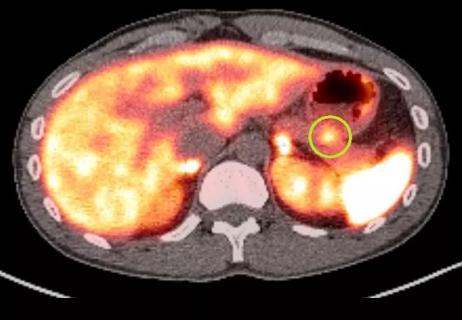
One critical issue is the variability of factors that can induce hyperglycemia in the hospital, including differences stemming from the illness or condition that brought the patient the patient in.
“How can we reduce rates of readmission for the patient with type one diabetes who’s in diabetic ketoacidosis (DKA)?” she says. “How do we prevent them from rebounding into the hospital? What about the patient with transplant-induced hyperglycemia, or steroid-induced hyperglycemia? How do we prevent them from needing to come back into the hospital due to their blood sugars?”
Advertisement
What is needed, she says, is a nuanced, multilayered set of evidence-based protocols to guide caregivers in the ER, intensive care, stepdown units, and as they prepare patients to go home or to be moved to long-term care.
“Rather than developing a specific way of administering medication, or a single technology for these transitional periods, we are focusing on processes to help prevent people from having to be readmitted,” she says.
Technology
The researchers soon will begin studying the effects of introducing continuous glucose monitoring (CGM) to patients with type 1 diabetes who are admitted with DKA. “We hope to reduce readmission by providing them with more data surrounding their glycemic control using CGM technology,” says Dr. Zhou.
Transplant patients
The team also is studying best practices for patients with diabetes who have had kidney transplants and are newly on high dose steroids followed by a taper. “How can we implement a specific insulin protocol that’s dependent on their steroid dose, other anti-rejection medications, and changing appetite, to actually help manage their hyperglycemia coming out the door?”
Similarly, she added, a team headed by Cecilia Lansang, MD, MPH, is working to develop computer algorithms that can design specific insulin protocols that can be used to bridge the gap in the care of kidney transplant patients on tapering doses of steroids. Proactive management of this transition is all the more important because, thanks to a collaboration between the kidney transplant team and endocrinologists, these patients are now able to be discharged between two and three days after surgery instead of five.
Teams
Dr. Zhou and her colleagues believe that coordinated teams and clearly outlined processes that can follow patients through these hospital transitions could improve outcomes by improving the care that patients receive.
Advertisement
The endocrinologists’ efforts build off previous work in which weight-based protocols were developed to more effectively transition hospitalized patients from IV insulin infusion to subcutaneously delivered insulin. In 2021, Drs. Lansang and Zhou, along with Mary T. Korytkowski, MD, at the University of Pittsburgh Medical Center, published Inpatient Hyperglycemia and Transitions of Care: A Systematic Review.1
The article highlighted the variability in care provided to patients with hyperglycemia in different physical locations within a hospital setting and at discharge and provides potential areas for further study.
1. Lansang MC, Zhou K, Korytkowski MT. Inpatient Hyperglycemia and Transitions of Care: A Systematic Review. Endocr Pract. 2021 Apr;27(4):370-377. doi: 10.1016/j.eprac.2021.01.016. Epub 2021 Jan 30. PMID: 33529732.
Advertisement
Advertisement
Patient’s unexplained low blood glucose levels in the absence of diabetes spark quest for answers

While results were negative for metformin, lifestyle counseling showed surprising promise
Rare genetic variant protected siblings against seizures and severe hypoglycemia

Maternal-fetal medicine specialists, endocrinologists and educators team up

Giving young patients a hand as they take charge of their own health

Case illustrates how easily condition can mimic preeclampsia

Analysis examines surgical resection of rare pituitary tumors

Building the bridge between endocrinology and geriatrics