How these findings remove some clinical subjectivity, guide management
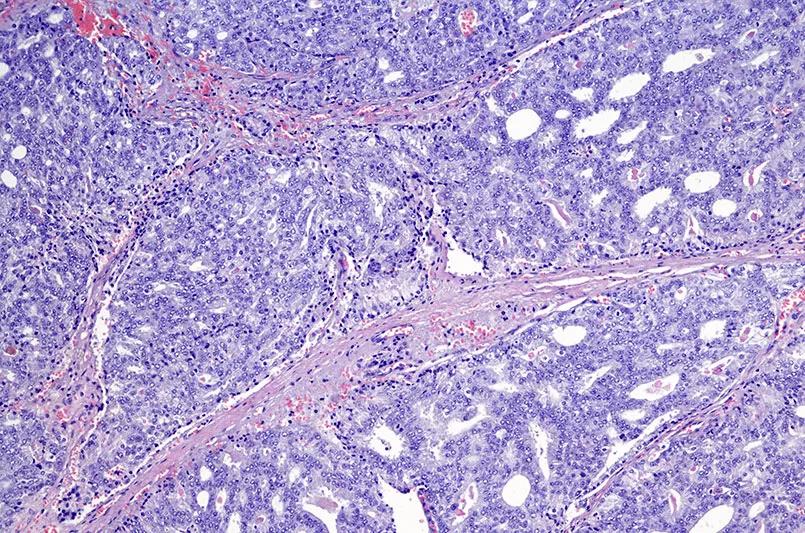
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3d60e663-7167-409b-a772-edb15a2d1596/650x450-Prostate-Cancer-Klein_jpg)
650×450-Prostate-Cancer-Klein
An assay used to determine cancer aggressiveness provided meaningful predictability associated with distant metastases (DM) and prostate cancer-specific mortality (PCSM), according to a study published in JCO Precision Oncology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The assay, known as Oncotype DX® Genomic Prostate Score (GPS), was developed by Cleveland Clinic researchers in partnership with Exact Sciences (formerly known as Genomic Health, Inc.) over a decade ago. The goal was to use high-end genomic technology, the same technology used to sequence the human genome, to identify molecular features of prostate cancer.
“This was the first time we created tools that allow us to directly assess the molecular architecture of early-stage prostate cancer in a way that it couldn’t be assessed before,” explains Eric Klein, MD, urologic oncologist and Chairman Emeritus of the Glickman Urological & Kidney Institute.
GPS is a diagnostic tool that allows urologic oncologists to personalize a patient’s course of treatment based on the tumor’s biology as measured by gene expression profiling. It helps identify candidates for active surveillance versus candidates for immediate therapy. Genomic testing – in conjunction with an MRI – is a standard of care in the evaluation of prostate cancer at Cleveland Clinic.
But the longer-term implications of these data points have been largely unknown — until recently. The JCO Precision Oncology study, led by Dr. Klein, is the first report to evaluate the predictive ability of GPS using long-term outcomes data.
Using a stratified cohort sampling method, the researchers examined 428 patients from 2,641 treated patients between 1987 and 2004. They looked at the GPS result assayed from radical prostatectomy tissue and compared it with the risk of DM and PCSM over 20 years following the procedure.
Advertisement
“Our findings revealed that lower GPS scores translate to a lower risk of metastases or prostate cancer-related mortality,” he says. “This should reassure physicians — and patients — that surveillance is safe.” Conversely, a higher score, above 29, is associated with a meaningful risk of metastasis or death.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/40c67047-85f7-45df-8a29-c6d0390babdd/805x-Inset-Oncotype-1_jpg)
Figure. RM-corrected estimates with 95% confidence intervals of the 20-year absolute risk of distant metastasis (A) and prostate cancer-specific mortality (B) as a function of the GPS result. GPS, Genomic Prostate Score; RM, regression to the mean. This figure was reprinted with permission from Wolters Kluwer Health, Inc. Brooks MA, Thomas L, Magi-Galluzzi C, et al. GPS assay association with long-term cancer outcomes: twenty-year risk of distant metastasis and prostate cancer–specific mortality. JCO Precis Oncol. Published online February 24, 2021. doi:10.1200/PO.20.00325
This study further solidifies genomic testing as a mainstay in the management of prostate cancer. Its ability to discriminate tumors’ molecular features can guide management strategies. Tumors with lower, more favorable scores can be carefully watched while higher, more concerning scores may warrant additional diagnostic procedures, closer follow-up or immediate treatment.
Dr. Klein says the data from this recent publication helps remove some clinical subjectivity. “These data indicate that decision-making can be dichotomized. Either you’re a good candidate for surveillance, or you’re not.”
He continues, noting that this study is more evidence that genomic tests provide clinically meaningful data. “The validity of these tests is well-documented, but we are starting to discover their clinical implications in the context of long-term outcomes — and this study shows the 20-year follow-up data to corroborate that.”
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality