Pilot study supports routine neuropsychological testing before and after the surgery
Patients who underwent an extended bifrontal approach for resection of a giant anterior cranial base meningioma had improved processing speed postoperatively and no significant changes in nine other neuropsychological quality-of-life (QOL) indicators in a Cleveland Clinic study presented at the 2019 annual meeting of the North American Skull Base Society.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Given the impairment we expect to see with frontal tumors, our findings suggest that the extended bifrontal approach may be an improvement over traditional surgery,” says Cleveland Clinic neurosurgeon Pablo Recinos, MD, senior author of the study. “Neuropsychological testing before and after brain surgery provided important information on quality-of-life parameters.”
Meningiomas are the most common intracranial neoplasm, representing about 40% of cases. Fortunately, WHO grade I meningiomas tend to have a benign course, especially after surgical resection. Often, however, patients have neuropsychological deficits from the tumor, and little is documented about how patients may improve — or worsen — as a result of surgery.
“Traditionally, success in brain tumor treatment is defined by extent of resection, as well as morbidity and mortality after surgery,” says Cleveland Clinic research team member Alankrita Raghavan, who presented the study. “However, because many patients with a meningioma live for decades after treatment, neuropsychological outcomes become a critically important consideration when determining the best surgical approach.”
She adds that QOL outcomes are especially relevant for a giant anterior base meningioma (defined as > 4 cm) because patients usually have considerable cognitive impairment preoperatively. Moreover, the surgery itself is not without risk, especially for such large tumors. Traditional bifrontal craniotomies can require significant brain retraction: Cortical infarction is more likely to occur when retraction pressures are above 20 mmHg and are held for longer than 15 minutes.
Advertisement
Reported outcomes in the literature with traditional surgery include significant postoperative impairments in neuropsychological measures, such as executive function, verbal memory and information processing.
The Cleveland Clinic researchers hypothesized that an extended bifrontal craniotomy would improve neuropsychological outcomes compared with the traditional approach. As shown in the photos below, extended bifrontal craniotomy involves removal of the orbital bar, thereby offering a low trajectory to the base of the tumor, decreasing the need for retraction and reducing edema because of the increased exposure.
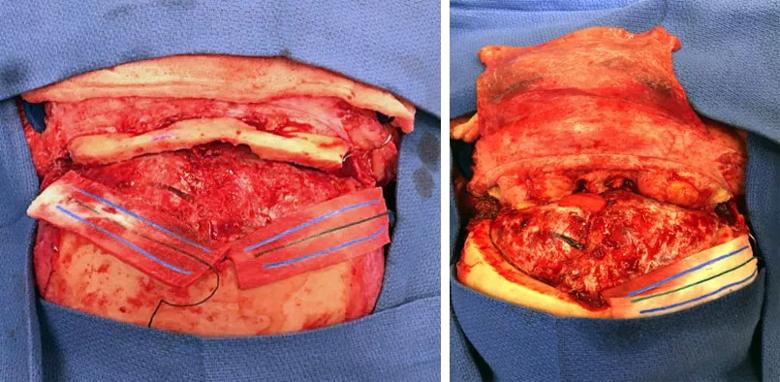
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a8d84846-a3c1-4ffe-b8a7-b06af113fe96/19-NEU-306-Recinos-Inset_jpg)
This pilot study involved 16 patients (10 women, mean age 56.3 years, mean tumor diameter 5.78 cm) who underwent an extended bifrontal craniotomy at Cleveland Clinic from 2016 through 2018. Traditional surgical parameters were evaluated, with 10 patients also undergoing neuropsychological assessment, which was designed and directed by neuropsychologist and coinvestigator Richard Naugle, PhD, of Cleveland Clinic’s Center for Behavioral Health.
Six patients had matched pre- and postoperative neuropsychological testing. Preoperative testing was usually performed within a few days of surgery; postoperative testing times varied (median, 90 days postoperatively [range, 84-112]).
The most common presenting symptoms preoperatively were cognitive changes (56%), personality changes (50%), anosmia (37.5%), visual deficits (37.5%) and seizures (25%).
Results of before-and-after neuropsychological testing were as follows:
Advertisement
In view of these findings, Dr. Recinos proposes assessing frontal lobe function in this patient population with a short battery of tests, consisting of:
Altogether, complete testing would take only about 40 minutes, he notes, while a standard battery of tests takes more than three times as long.
Dr. Recinos adds that the proposed tests are not the most challenging in each domain. If a patient performed particularly poorly in any area, further specific testing could be done to ascertain a more precise score.
“The results of our small study demonstrate the need for efficient and effective neuropsychological testing that can be routinely administered to evaluate standard and novel surgical approaches,” concludes Dr. Recinos. “Such testing could also help us inform patients which parameters can be expected to change after surgery and which areas may require postoperative rehabilitative therapy.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units