New study examines rates of downgrading in patients with aggressive prostate cancer
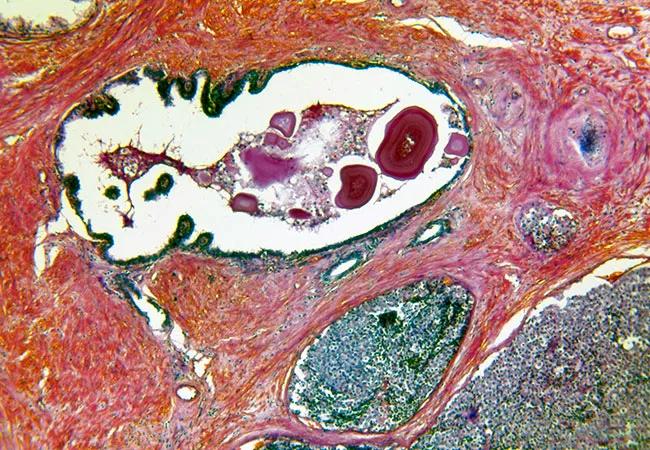
For most cancers, the nuclei of the cancer cell are indicative of how aggressive the malignancy is. In prostate cancer, however, the shape and configuration of the cells that make up each individual gland, rather than the nucleus, provides a better basis for diagnosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recognizing this, the Gleason scoring system, implemented in the 1970s, assesses both the appearance of the cells — ranging from more to less disordered — and also includes the sum of primary and secondary cell patterns. Often in prostate cancer, more than one pattern is present.
This heterogeneous cell pattern and growth can understandably lead to inaccuracies in prostate biopsies. A needle biopsy may capture a particularly high- or low-grade pattern that does not reflect the true nature of the malignancy. In fact, a closer evaluation of the specimen after prostatectomy may lead physicians to change the patient’s risk category altogether, known as upgrading or downgrading.
Investigators recently led a study to better assess the rate of downgrading in a cohort of patients with high-grade prostate cancer on initial biopsy. They reported their findings in the Journal of Urology.
Eric Klein, MD, Chair of Glickman Urological & Kidney Institute and co-author of the study, remarks, “Accurate risk stratification is critical for treatment planning and management of patient expectations.” He continues, “We hoped to determine how often a high-grade biopsy actually translated to high-grade disease or if it was the result of a sampling error.”
The study examined 1,776 men with localized high risk (PSA >20 ng/ml, Grade Group (GG) 4-5, or clinical stage ≥ T3) or very high risk (primary Gleason pattern 5, more than four biopsy cores with GG 4-5, or two or more HR features) prostate cancer who underwent radical prostatectomy (RP) from 2005 to 2015. Investigators examined patients diagnosed with GG 4 disease at the time of biopsy and had data available for analysis (N = 726).
Advertisement
Of this cohort, 45% of patients (N = 333) were downgraded to GG ≤ 3 after surgery. This is significantly lower than similar studies that have approximated as many as 60% of high-grade cases may be downgraded. Of these, 16% (98/604) of high-risk patients and 7% (8/122) of very high-risk patients (P < 0.01) were downgraded to GG ≤ 2.
Downgraded patients shared the following clinical and oncological traits. The majority of downgraded biopsies had Gleason pattern 4+4 (86.7%), as compared to 3+5 or 5+3 (P = 0.003). On average, they also had lower PSA levels, fewer positive biopsy cores and lower clinical stage. Taken together, this data may give clinicians evidence to predict whether a biopsy is likely to be downgraded following RP.
“In other words, if a patient shows a high-risk or very high-risk cancer on biopsy, there is a good chance that it is, in fact, a high-grade malignancy, and is fine to proceed with a more aggressive treatment plan,” says Dr. Klein.
And while it’s unlikely that a biopsy downgrade from GG 4 to GG 3, for example, would have altered the course of treatment in a significant way, the psychological implications for patients and the difference in prognosis discussions should not be overlooked.
“Our findings affirm that despite some challenges with high-grade prostate cancer biopsy, we can still be relatively confident that the diagnosis is consistent with final pathology,” comments Dr. Klein. “This is just one more way to help manage care for patients and counsel them on treatment.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units